Latest Blogs
Pneumonitis: Causes, Symptoms, and How to Treat This Lung Condition
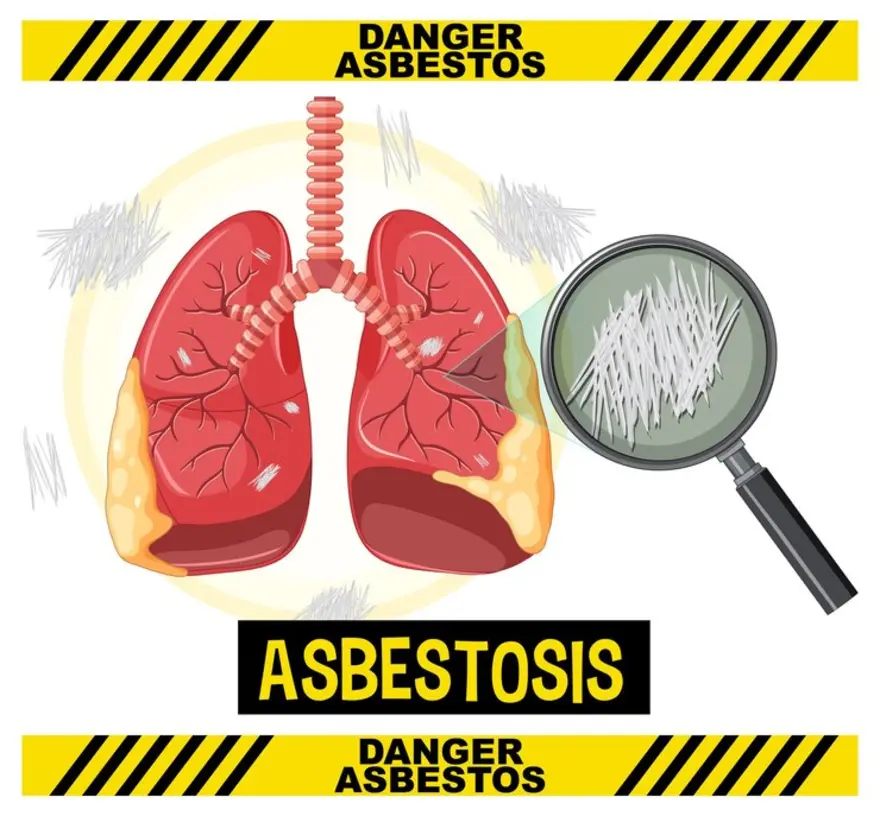
What is pneumonitis? Pneumonitis is a lung inflammation caused by an immune reaction to an irritant, not an infection. When the tiny air sacs in the lungs (alveoli) become swollen and inflamed, it becomes harder for oxygen to pass into the bloodstream. This can lead to breathing difficulties, coughing and other respiratory symptoms. Is pneumonitis serious? Left untreated, pneumonitis can indeed become a serious health issue. Ongoing lung inflammation can result in permanent scarring and damage called pulmonary fibrosis. Chronic pneumonitis may also cause complications like substantial weight loss, clubbing (enlargement) of the fingers and toes, and significantly reduced lung function. Prompt diagnosis and pneumonitis treatment are important to prevent the condition from progressing to this stage. What are the types of pneumonitis? Pneumonitis can be classified into various types based on the underlying cause, each with distinct characteristics. By recognising the various pneumonitis types, healthcare providers can tailor their approach to improve patient outcomes. Hypersensitivity Pneumonitis (HP) is the most common type and results from an allergic reaction to inhaled organic dust, molds, chemicals, or other substances. It can present as either acute or chronic, depending on exposure and individual sensitivity. Drug-induced Pneumonitis occurs as a side effect of certain medications, including some antibiotics, chemotherapy drugs, and heart medications. This type can vary in severity and duration based on the specific drug involved. Radiation Pneumonitis may develop in patients undergoing radiation therapy to the chest, such as for breast or lung cancer. Understanding these pneumonitis types is crucial for effective diagnosis and treatment, as each requires different management strategies. What are the symptoms of pneumonitis? Pneumonitis symptoms can vary depending on whether the condition is acute or chronic. Signs of acute pneumonitis, which usually appear 4-6 hours after exposure to the triggering substance, often include: Fever and chills Muscle or joint pain Headache Chronic pneumonitis symptoms develop more gradually and are characterised by: Dry cough Chest tightness or pain Fatigue Decreased appetite and weight loss Shortness of breath, especially with activity What causes pneumonitis? Pneumonitis causes center around the inhalation of substances that provoke an exaggerated immune response in the lungs. Some of the most common triggers include: Molds and bacteria (e.g. in humidifiers, air conditioners, hot tubs) Bird droppings or feathers (called bird fancier's lung) Dust from animal fur, hardwood, or metal particles Grains and hay containing mold spores (farmer's lung) Chemicals (e.g. pesticides, aerosolised mists) Certain medicines (chemotherapy drugs, antibiotics, etc.) Radiation therapy to the chest Is pneumonitis contagious? You can rest assured that pneumonitis itself is not contagious. Since it stems from an individual's immune reaction to a particular substance rather than an infection, you cannot "catch" pneumonitis from someone else. Who does pneumonitis affect? Pneumonitis can develop in people of any age, but the average age at diagnosis is between 50 to 55 years old. You may be at higher risk if you have a family history of the condition. Frequent exposure to organic dust, molds, chemicals or other irritants - whether at work, at home or through hobbies - also makes a person more prone to pneumonitis. What are the complications of pneumonitis? If pneumonitis progresses without proper treatment, it can lead to serious complications such as: Pulmonary fibrosis, which causes irreversible scarring of the lung tissue Severe weight loss and systemic symptoms Clubbing of fingers and toes due to chronic lung disease Respiratory failure in very severe cases How is pneumonitis diagnosed? To diagnose pneumonitis, your doctor will start by taking a thorough medical history, asking about your symptoms and any exposure to potential irritants. This will be followed by a physical exam to check for abnormal lung sounds. What tests will be done to diagnose pneumonitis? To diagnose pneumonitis, several tests are performed to assess lung inflammation and rule out other conditions. Chest X-ray and CT scans are essential imaging techniques that help identify signs of lung inflammation. These scans can reveal the extent and pattern of damage. Spirometry is another important test used to assess lung function, measuring how much air you can inhale and exhale, which can indicate the severity of the condition. Pulse oximetry or arterial blood gas tests measure blood oxygen levels, providing insight into how well the lungs are functioning. Bronchoscopy allows doctors to visually examine the lungs and collect samples of tissue or fluid for further analysis. Finally, a lung biopsy may be conducted to analyze lung tissue under a microscope. Understanding the pneumonitis causes is vital for appropriate pneumonitis treatment, as different pneumonitis types may require tailored therapeutic approaches to manage symptoms effectively. How is pneumonitis treated? Pneumonitis treatment focuses on reducing lung inflammation and preventing further exposure to the triggering substance. The specific approach depends on the severity of your symptoms. Mild cases may get better on their own after avoiding the irritant Oral corticosteroids are used to control inflammation in more serious cases Oxygen therapy may be needed if blood oxygen levels are low Immunosuppressant drugs may be prescribed if steroids are ineffective In addition, your doctor will advise you to: Identify and strictly avoid any substances that triggered the pneumonitis Quit smoking and avoid exposure to secondhand smoke Get plenty of rest to help your body recover Stay well-hydrated and eat a balanced diet to support healing How soon after treatment will I feel better? With proper pneumonitis treatment, most people start to feel better within a few days to weeks. The full recovery time varies depending on the extent of inflammation. Chronic pneumonitis usually improves within 2-3 months, provided the lungs have not been severely scarred. Your doctor will monitor your progress through regular follow-up visits and tests. How to prevent pneumonitis? While not all cases are preventable, you can reduce your pneumonitis risk by taking these precautions: Minimise exposure to known triggers like dust, mold, chemicals and smoke Wear a face mask when working with hay, wood dust or other irritants Make sure indoor spaces are well-ventilated Review your medications with your doctor to identify any that may cause pneumonitis What is the outlook for pneumonitis? With early diagnosis and proper treatment, the outlook for pneumonitis is generally good. The condition often resolves fully if the lungs have not been permanently damaged. Identifying and avoiding triggers is key to preventing relapses. In chronic cases, ongoing monitoring and medication may be needed to manage symptoms and slow disease progression. Severe cases that cause lung scarring may have a poorer prognosis. How long does pneumonitis last? The duration of pneumonitis varies depending on the cause, severity and individual factors. Acute pneumonitis often clears up within a few days to weeks once the trigger is removed. Chronic cases usually improve within 3 months with treatment, but some people may have ongoing symptoms if lung scarring has occurred. Your healthcare provider can give you a better estimate based on your specific condition. Can you fully recover from pneumonitis? Yes, complete recovery from pneumonitis is possible, especially if the condition is diagnosed and treated promptly before permanent lung damage occurs. However, if significant scarring has developed, lung function may be compromised long-term and some symptoms may linger. Following your treatment plan and taking steps to avoid triggers can improve your chances of a full recovery. When to see a doctor for pneumonitis? It's important to consult your healthcare provider if you experience symptoms suggestive of pneumonitis, such as shortness of breath, cough, fever and fatigue - especially if you have been exposed to any known triggers. Identifying and treating pneumonitis early helps prevent complications. If you have been diagnosed with pneumonitis, see your doctor promptly if your symptoms suddenly worsen or do not improve with treatment. What is the difference between pneumonia and pneumonitis? While both pneumonia and pneumonitis involve lung inflammation and similar symptoms, they differ in their causes. Pneumonia is triggered by an infection with bacteria, viruses or fungi, while pneumonitis is a non-infectious condition caused by exposure to an irritating substance. Pneumonia is treated with antibiotics, whereas pneumonitis treatment focuses on reducing inflammation and avoiding triggers. Conclusion Being diagnosed with pneumonitis can feel overwhelming, but understanding the condition is an empowering first step in regaining control of your health. Identifying and avoiding your unique triggers, along with following your doctor's treatment plan, goes a long way towards managing symptoms and preventing complications. If you need support or have questions, don't hesitate to talk to your healthcare provider. You can also explore reputable online resources like Metropolis Healthcare's website for more information on lung health and diagnostic testing services. Remember, with the right knowledge, care and lifestyle adjustments, you can breathe easier and get back to living your fullest life.
Proctitis: Causes, Symptoms, and Treatment for Rectal Inflammation
What is proctitis? Proctitis refers to inflammation of the mucosal lining of the rectum, the final segment of the large intestine connecting the colon to the anus. When the rectal lining becomes inflamed, it can cause various uncomfortable symptoms related to bowel movements and rectal discomfort. Proctitis can occur as an acute condition, meaning it comes on suddenly and lasts for a short time, or it can be chronic, persisting for an extended period. Understanding proctitis causes is essential for effective treatment, as inflammation can arise from various factors. What are the different types of proctitis? There are several proctitis types, each with distinct characteristics: Proctitis associated with Inflammatory Bowel Disease (IBD) is linked to chronic conditions like ulcerative colitis and Crohn's disease. Infectious Proctitis is caused by STIs and other infections like Salmonella. Radiation Proctitis results from radiation therapy, while Diversion Proctitis occurs post-ostomy surgery. The risk factors and severity can vary depending on individual circumstances. Understanding these proctitis types is crucial for effective management. What are the symptoms of proctitis? The proctitis symptoms you experience may vary depending on the underlying cause and severity of your condition. Common signs of proctitis symptoms include: A constant urge to have a bowel movement, even when the bowel is empty Changes in bowel habits, with stools being either loose and watery or hard and difficult to pass Cramping, tenderness, or pain in the anus, rectum, or left side of the abdomen Passing blood, mucus, or pus along with stool What are the first signs of proctitis? The initial proctitis symptoms typically appear during bowel movements and may include: Tenderness, burning, or cramping when trying to have a bowel movement Urgent need to defecate Loose stools, blood in the stool, or mucus being passed along with stools What are the causes of proctitis? Proctitis, an inflammation of the rectum lining, can be caused by a variety of factors, each impacting treatment options and symptom management. Let’s look at some common and less common causes of proctitis. Common proctitis causes of proctitis include: Inflammatory Bowel Disease (IBD): Chronic digestive disorders such as ulcerative colitis and Crohn’s disease can cause proctitis as part of their range of symptoms. These conditions frequently lead to recurring inflammation, pain, and even bleeding in the rectum. Managing IBD-related proctitis often requires long-term treatment, including anti-inflammatory medications and lifestyle modifications. Sexually Transmitted Infections (STIs): Some STIs, including gonorrhoea, herpes, chlamydia, and lymphogranuloma venereum, can infect the rectum, causing significant inflammation. This proctitis type, often seen in individuals who engage in anal intercourse, can lead to discomfort and rectal pain. Prompt diagnosis and treatment with appropriate antibiotics or antivirals can resolve symptoms and prevent complications. Radiation Therapy: Radiation treatment for cancers in the pelvic region, such as cervical, prostate, or rectal cancer, can cause radiation proctitis. Radiation proctitis is a common side effect due to rectal lining damage from radiation exposure. Symptoms like chronic inflammation, bleeding, and bowel habit changes may persist, requiring specialised therapies for symptom relief. Infections: Non-sexually transmitted bacterial infections such as Salmonella, Shigella, and Clostridioides difficile (C. diff) can also lead to proctitis. These infections, particularly in individuals with compromised immune systems, can result in rectal inflammation that needs targeted antibiotic treatment to prevent further complications. Ostomy Surgery: In patients with an ostomy (where part of the intestine empties through the abdominal wall), a remaining rectal stump can develop inflammation, known as diversion proctitis. Managing diversion proctitis may involve medications or other therapies. Some less common proctitis causes include: Anal Injuries: Injuries from anal sex or anal play may lead to inflammation and discomfort, potentially causing proctitis if the tissue is irritated or damaged. Medications: Certain medications, particularly NSAIDs, have been linked to proctitis as a side effect. In these cases, changing or stopping the medication under medical guidance may relieve symptoms. Insertion of Harmful Substances: The introduction of foreign or harmful substances into the rectum can damage tissues and lead to inflammation. Autoimmune Diseases: Other autoimmune conditions, like lupus, may cause autoimmune proctitis, where the immune system mistakenly attacks rectal tissue. Proctitis severity can vary greatly depending on the underlying cause, making an accurate diagnosis essential for effective treatment and symptom management. Is proctitis a serious condition? Proctitis can be a serious condition if it is left untreated or if it leads to complications. Potential complications of proctitis include: Severe rectal bleeding Narrowing of the rectum (stricture) due to scarring Development of abscesses or abnormal passageways (fistulas) around the rectum Anaemia from chronic blood loss Increased risk of infections However, with timely diagnosis and appropriate treatment, the prognosis for proctitis is generally good. Most people are able to manage their symptoms effectively and prevent serious complications. How is proctitis diagnosed? If your doctor suspects proctitis, they will perform a series of diagnostic steps to confirm the condition and identify the underlying cause. This helps guide appropriate proctitis treatment based on each individual’s needs. The diagnostic process typically involves: Medical History: Your doctor will begin by asking about your symptoms, sexual history, previous medical conditions, medications, and any history of radiation therapy or ostomy surgery. This information provides a crucial background for understanding potential causes of proctitis. Physical Exam: A comprehensive physical examination, including a digital rectal exam, is usually performed. This allows the doctor to check for inflammation, bleeding, or masses in the rectum. Tests: Depending on your case, several tests may be recommended, including: Blood Tests: These assess levels of inflammation or infection indicators, helping to identify underlying causes. Stool Tests: Stool samples are examined for infectious organisms like bacteria, viruses, or parasites, which can be contributing factors. Rectal Culture: For cases where sexually transmitted infections (STIs) are suspected, a rectal culture is done to detect specific pathogens. Endoscopic Procedures: Procedures such as flexible sigmoidoscopy or colonoscopy allow direct visualization of the rectum. During these procedures, a tissue biopsy may be taken to provide more precise information about the type and extent of inflammation. Accurate diagnosis is essential to selecting an effective proctitis treatment plan tailored to the cause and severity of the condition. Does proctitis go away by itself? Proctitis usually requires treatment and does not resolve on its own. The type and duration of treatment depend on the underlying cause of your proctitis. For example: Infectious proctitis caused by STIs or bacteria typically requires antibiotics. Proctitis related to IBD often requires anti-inflammatory medications and immunosuppressants. Radiation proctitis may improve on its own over time, but some people need treatments like laser therapy or medications to control bleeding. Diversion proctitis usually resolves after surgery to reconnect the ostomy. How long does proctitis last? The duration of proctitis depends on the underlying cause and the effectiveness of treatment. Some cases of infectious proctitis may resolve within a few weeks with antibiotics, while proctitis related to chronic conditions like IBD may require long-term management. Working closely with your healthcare provider can help you control your symptoms and minimise the impact of proctitis on your daily life. What is the treatment for proctitis? Proctitis treatment depends on the underlying cause. Options include antibiotics for bacterial infections, anti-inflammatory drugs for IBD-related cases, immunosuppressants for severe inflammation, and laser therapy or electrocautery for radiation proctitis. In severe cases, surgery may be necessary. Your doctor tailors treatment to your needs. How to prevent proctitis? While not all cases of proctitis can be prevented, there are some steps you can take to lower your risk: Practice safe sex If you have IBD, work with your doctor to keep your condition well-controlled with medications and lifestyle changes. Be cautious with anal sex or anal play to avoid injuring the rectum. Take NSAIDs only as directed and consider alternatives if you're prone to digestive issues. Don't insert harmful substances into the rectum. What is the outlook for proctitis? With proper treatment, the outlook for proctitis is generally positive. Acute cases often resolve within weeks to months, while chronic proctitis linked to IBD can be managed with medication and lifestyle changes to control symptoms. Regular follow-ups help ensure effective management, allowing most individuals to maintain a good quality of life. When to see a doctor about proctitis? Seek medical attention for proctitis symptoms like rectal pain, changes in bowel habits, blood, mucus, or pus in stool, tenesmus, or fever. Prompt diagnosis aids in effective treatment and prevents complications. Mention any history of IBD, STIs, pelvic radiation, or ostomy surgery to help guide your doctor’s evaluation. Conclusion Dealing with proctitis can be challenging, but with the right knowledge and care, it's possible to manage your symptoms and maintain good rectal health. If you suspect you may have proctitis, don't hesitate to consult your healthcare provider for personalized guidance and treatment options. At Metropolis Healthcare, we understand the importance of accurate diagnosis in managing conditions like proctitis. Our team of skilled technicians offers convenient at-home sample collection services, ensuring your tests are processed promptly at our state-of-the-art labs. With reliable results and expert support, we're committed to empowering you to take control of your health.
Cholangiocarcinoma: Understanding Bile Duct Cancer and Treatment Options
What is cholangiocarcinoma (bile duct cancer)? Cholangiocarcinoma, or bile duct cancer, arises from the cells lining the bile ducts - the tubes that carry bile from the liver to the small intestine to aid in fat digestion. This uncommon cancer can develop in any part of the bile duct system. The bile ducts include: Intrahepatic ducts: Small ducts within the liver Extrahepatic ducts: Ducts outside the liver, including the common hepatic duct and common bile duct Perihilar ducts: The area where the right and left hepatic ducts join to form the common hepatic duct What are the types of bile duct cancer? Cholangiocarcinoma types are defined based on their location in the bile duct system, and each type has distinct characteristics affecting diagnosis and treatment strategies. Intrahepatic cholangiocarcinoma: This type arises within the liver’s bile ducts, representing about 10% of all bile duct cancers. It can be challenging to diagnose as it resembles liver cancer in appearance and symptoms. Perihilar (hilar) cholangiocarcinoma: The most common cholangiocarcinoma type, developing at the junction where the right and left hepatic ducts meet, accounting for 50-60% of cases. Distal cholangiocarcinoma: Occurs in the bile ducts outside the liver, closer to the small intestine, making up 20-30% of all cases. Recognising these cholangiocarcinoma types is essential for effective treatment planning and prognosis. How common is cholangiocarcinoma? Cholangiocarcinoma, or bile duct cancer, is a rare cancer, accounting for only 3% of all gastrointestinal malignancies. The global incidence varies, with the highest rates in Southeast Asian countries like Thailand due to risk factors like liver fluke infections. In the US, approximately 8,000 people are diagnosed with bile duct cancer each year. What are the symptoms of cholangiocarcinoma? Cholangiocarcinoma symptoms often go unnoticed in the early stages, as they may not appear until the tumour grows and obstructs the bile ducts. As it progresses, common signs include: Jaundice (yellowing of the skin and eyes) Itchy skin Light-colored, greasy stools Dark urine Upper right abdominal pain Unintended weight loss Fever Nausea and vomiting If you experience any of these cholangiocarcinoma symptoms, consult your doctor promptly. While these signs don't confirm bile duct cancer, they warrant further investigation, as similar symptoms can arise from other health issues. What causes cholangiocarcinoma? The exact cholangiocarcinoma causes are not fully understood, but experts believe a combination of genetic and environmental factors may be involved: Chronic inflammation of the bile ducts due to conditions like primary sclerosing cholangitis (PSC) Exposure to certain chemicals and toxins Liver fluke parasitic infections (mainly in Asia) Genetic mutations in genes like TP53, KRAS, SMAD4 and IDH1/2 In most cases, cholangiocarcinoma occurs in people with no known risk factors, so having one doesn't mean you will develop the disease. What are the risk factors of cholangiocarcinoma? Some factors that may increase the likelihood of developing cholangiocarcinoma include: Primary sclerosing cholangitis (PSC): Chronic inflammation of bile ducts Liver fluke infections: Parasites like Opisthorchis viverrini and Clonorchis sinensis Choledochal cysts: Congenital bile duct abnormalities Hepatitis B or C viral infection Cirrhosis (scarring) of the liver Obesity Older age (over 60 years) Smoking Excessive alcohol use Family history of the disease Having any of these risk factors doesn't mean you'll get bile duct cancer, and many people with cholangiocarcinoma have no known risk factors. However, if you have PSC or other risk factors, your doctor may recommend regular screening. How is cholangiocarcinoma diagnosed? Diagnosing cholangiocarcinoma requires a comprehensive approach to determine its presence, type, and extent, beginning with a medical history and physical examination. Your doctor will ask about symptoms, risk factors, and any history of liver conditions, checking for signs like jaundice, abdominal pain, and tenderness. Blood Tests: Liver function tests assess levels of bilirubin and liver enzymes, which may be elevated if the bile ducts are obstructed. Tumour markers such as CA 19-9 and CEA are sometimes elevated in bile duct cancer, though they are not definitive alone. Imaging Tests: Ultrasound provides an initial look at the liver, bile ducts, and nearby organs. CT scans can help locate tumours and identify potential spread to nearby tissues. MRI with MRCP (magnetic resonance cholangiopancreatography) gives detailed images of bile ducts, showing any blockages or abnormalities. PET scans can detect cancer spread to lymph nodes or distant organs. Diagnostic Procedures: ERCP (endoscopic retrograde cholangiopancreatography) allows doctors to view bile ducts, collect samples, and place stents if ducts are blocked. PTC (percutaneous transhepatic cholangiography) is a procedure in which a dye is injected into the bile ducts to visualise blockages on X-rays. A tissue sample may be obtained through fine-needle aspiration (FNA), core biopsy, or during ERCP/PTC. Examining this sample under a microscope confirms the diagnosis. An accurate diagnosis is essential for staging cholangiocarcinoma and creating an effective treatment plan. Early testing is especially important for those at high risk. How is cholangiocarcinoma staged? Cholangiocarcinoma staging assesses the size and spread of the cancer to guide treatment decisions and prognosis. The most common staging system for bile duct cancer is the TNM system: T (Tumour): Size and extent of the main tumour N (Nodes): Spread to nearby lymph nodes M (Metastasis): Spread to distant organs like the lungs, bones or brain Based on TNM scores, cholangiocarcinoma is assigned a stage from 0-4: Stage 0: Precancerous changes in bile duct cells Stage 1: Cancer is confined to the bile duct Stage 2: Cancer has grown through the bile duct wall Stage 3: Cancer has spread to nearby lymph nodes or structures Stage 4: Cancer has metastasized to distant organs In general, earlier stages have a better prognosis and more treatment options than advanced stages. Your doctor can explain your individual stage and what it means for your care plan. How is cholangiocarcinoma treated? Cholangiocarcinoma treatment is tailored to individual circumstances, influenced by the cancer’s location, stage, and the patient's overall health. Early-stage cholangiocarcinoma may be eligible for curative surgical options, which include various procedures such as resection, hepatectomy, and the Whipple procedure. These surgeries aim to remove the affected bile duct and, in some cases, parts of the liver, gallbladder, or pancreas. For some patients, particularly those with early perihilar cholangiocarcinomas, a liver transplant may be considered. However, this option requires extensive evaluation and adherence to strict medical criteria. In cases where surgery isn’t possible, chemotherapy can be a vital component of cholangiocarcinoma treatment. Chemotherapy uses powerful drugs, such as gemcitabine, cisplatin, and 5-fluorouracil, to destroy cancer cells. It can also help shrink tumours before surgical procedures or control the disease in advanced stages. Radiation therapy is another option, utilising high-energy beams to target and kill cancer cells in specific areas. This treatment can also relieve symptoms like pain and blockages. Emerging treatments like targeted therapy and immunotherapy offer new avenues for patients. Targeted therapy, such as pemigatinib, focuses on specific genetic changes in cancer cells, while immunotherapy, including pembrolizumab, leverages the immune system to combat cancer. Clinical trials present opportunities for patients to access novel therapies that are still under investigation. Additionally, palliative care focuses on symptom relief and improving the quality of life, complementing other treatments at any stage of the disease. Your healthcare team will create a personalised cholangiocarcinoma treatment plan to address your specific needs. Always feel empowered to ask questions, seek second opinions, and gather support throughout your treatment journey. How can we prevent cholangiocarcinoma? While there's no sure way to prevent cholangiocarcinoma or bile duct cancer, you can lower your risk by: Treating parasitic liver fluke infections promptly Managing conditions like PSC and hepatitis with your doctor's guidance Avoiding harmful chemicals and toxins Maintaining a healthy weight through diet and exercise Limiting alcohol intake Avoiding smoking or using tobacco products What is the outlook for cholangiocarcinoma? The prognosis for cholangiocarcinoma depends on factors like the tumour location, stage at diagnosis, treatment response and your overall health. In general, the earlier the cancer is caught, the better the outcome. Survival rates for bile duct cancer are: Localised (no spread): 25% alive at 5 years Regional (spread to nearby structures): 7% alive at 5 years Distant (spread to distant organs): 2% alive at 5 years How curable is bile duct cancer? Bile duct cancer is potentially curable when caught at an early stage before it spreads. Depending on the tumour type and location, surgery to remove the cancer offers the best chance for long-term survival. However, many cholangiocarcinomas are diagnosed at a later stage when a cure may no longer be possible. In these cases, treatment focuses on controlling the cancer, relieving symptoms and maintaining quality of life for as long as possible. Conclusion Being diagnosed with cholangiocarcinoma is undoubtedly challenging, but understanding more about this disease is an important first step. If you're concerned about your risk for cholangiocarcinoma or are experiencing potential symptoms, don't delay seeking medical advice. Trusted diagnostic labs like Metropolis Healthcare offer comprehensive blood tests and health check-ups to empower you in monitoring your well-being.
Primary Biliary Cholangitis: Early Detection and Management Strategies
What is primary biliary cholangitis? Primary biliary cholangitis (PBC) is a chronic autoimmune liver disease characterised by the gradual destruction of the intrahepatic bile ducts. These small ducts are responsible for transporting bile from the liver to the small intestine, which aids digestion and absorption of fats and fat-soluble vitamins. In PBC, the immune system mistakenly attacks and damages these ducts, causing inflammation, scarring, and eventual blockage. What does "primary biliary cholangitis" mean? The term "primary biliary cholangitis" refers to the primary involvement of the intrahepatic bile ducts and the inflammatory process (cholangitis) that affects them. "Primary" indicates that the condition originates within the liver, rather than secondary to another underlying cause. "Biliary" pertains to the bile ducts, while "cholangitis" describes the inflammation of these ducts. How does primary biliary cholangitis affect our body? Primary biliary cholangitis affects the body by disrupting bile flow due to immune damage in liver ducts, causing bile buildup and inflammation. This can cause fibrosis and eventually cirrhosis, impairing liver function. Common primary biliary cholangitis symptoms include fatigue, itching, jaundice, and abdominal discomfort, along with nutrient deficiencies from impaired fat and vitamin absorption. Is primary biliary cholangitis serious? Yes, primary biliary cholangitis is a serious progressive disease that, if left untreated, can lead to severe complications and even liver failure. While the course of PBC varies among individuals, it typically advances slowly over many years. However, in some cases, the disease can progress rapidly, causing extensive fibrosis and cirrhosis within a shorter timeframe. Studies suggest that up to 30% of patients may experience a more aggressive form of PBC, underscoring the importance of early diagnosis and proactive management. What is the difference between primary biliary cholangitis vs. primary sclerosing cholangitis? Primary biliary cholangitis (PBC) and primary sclerosing cholangitis (PSC) are chronic autoimmune liver diseases affecting bile ducts but differ in scope. PBC targets small ducts within the liver, mostly in women, while PSC impacts both intrahepatic and extrahepatic ducts, affecting men more. PBC is often treatable with UDCA or OCA, whereas PSC lacks proven treatments, focusing instead on symptom management. Who does primary biliary cholangitis affect? PBC predominantly affects women aged 35–60, with primary biliary cholangitis causes likely involving hormonal factors, genetic predisposition, and environmental triggers. It often clusters within families, suggesting a genetic link, with first-degree relatives at higher risk. Primary biliary cholangitis diagnosis is important as it can occur at any age or gender, so individuals should watch for liver-related symptoms and consult healthcare providers when concerned. What are the symptoms of primary biliary cholangitis? Primary biliary cholangitis symptoms can vary from person to person and may not be present in the early stages of the disease. Many individuals are diagnosed incidentally through routine blood tests that reveal elevated liver enzymes, particularly alkaline phosphatase (ALP). As the disease progresses, the following symptoms may develop: Fatigue: Persistent, unexplained tiredness that doesn't improve with rest is one of the most common primary biliary cholangitis symptoms, affecting up to 80% of patients. This fatigue can be debilitating and significantly the impact quality of life. Pruritus (itching): Intense, persistent itching, often worse at night, is an another frequent symptom. The itching may be localised or widespread and can be severe enough to cause sleep disturbances and skin damage from scratching. Abdominal pain: Some individuals may experience discomfort or pain in the upper right part of the abdomen, where the liver is located. This pain may be dull, aching, or even sharp at times. Jaundice: As the disease advances and bile builds up in the liver, bilirubin levels rise, causing a yellowing of the skin and whites of the eyes. Jaundice is often a sign of more advanced PBC. Dry eyes and mouth: PBC is often associated with other autoimmune conditions, such as Sjögren's syndrome, which can cause dryness of the eyes (sicca syndrome) and mouth (xerostomia). Osteoporosis: The malabsorption of vitamin D and calcium due to impaired bile flow can lead to thinning of the bones (osteoporosis), increasing the risk of fractures. What are the complications of biliary disease? Biliary disease can lead to several complications, primarily due to impaired bile flow, which affects digestion and liver function. Fat Malabsorption Biliary disease impairs bile production or flow, which is essential for breaking down and absorbing fats in the intestine. When bile is insufficient, the body struggles to digest dietary fats and absorb fat-soluble vitamins like A, D, E, and K. This malabsorption can lead to nutrient deficiencies with symptoms including night blindness (from vitamin A deficiency), bone thinning and fractures (from vitamin D deficiency), poor immune function (from vitamin E deficiency), and issues with blood clotting (from vitamin K deficiency). Over time, fat malabsorption can also contribute to weight loss, muscle weakness, and overall nutrient depletion, which can significantly impact health and energy levels. Portal Hypertension Biliary disease, especially if it progresses to advanced liver scarring (cirrhosis), can lead to portal hypertension. This condition occurs when scarring obstructs blood flow through the liver, increasing pressure in the portal vein. Complications from portal hypertension can include varices (swollen veins) in the oesophagus and stomach, which pose a high risk of bleeding, as well as fluid buildup in the abdomen (ascites) and spleen enlargement (splenomegaly). Managing these complications typically requires specialised treatments to reduce risks and maintain quality of life. What causes primary biliary cholangitis? Primary biliary cholangitis causes remain unclear, but research indicates a combination of genetic predisposition and environmental factors. Genetics play a significant role; individuals with a family history of PBC are at higher risk, and studies suggest certain immune-regulating genetic variations may increase susceptibility. However, these genetic markers alone don’t guarantee disease onset, highlighting the role of environmental triggers in primary biliary cholangitis causes. Possible triggers include infections, like Escherichia coli, where molecular mimicry may lead the immune system to mistakenly attack bile duct cells. Other potential risk factors include exposure to environmental toxins, such as cigarette smoke, and certain medications. Importantly, PBC is not caused by alcohol or hepatitis and cannot be transmitted between individuals, remaining a non-contagious autoimmune condition. How is primary biliary cholangitis diagnosed? Primary biliary cholangitis diagnosis is a detailed process involving multiple steps to confirm the disease and assess its progression. Medical History and Physical Exam The diagnostic process begins with a thorough review of medical history, including any symptoms, family history, and other conditions. During the physical exam, a doctor will check for signs of liver disease, such as jaundice, an enlarged liver, or other physical symptoms that may indicate liver involvement. Blood Tests Antimitochondrial Antibodies (AMA): A key diagnostic marker, AMAs are present in over 90% of PBC cases and strongly indicate the disease. Liver Function Tests: Elevated alkaline phosphatase (ALP) and gamma-glutamyl transferase (GGT) levels are common indicators in PBC patients, suggesting bile duct damage or obstruction. Additional Tests: Complete blood count (CBC), bilirubin, albumin, and prothrombin time help assess liver function and determine the stage of the disease, as well as any progression. Imaging Tests Ultrasound, CT scans, or MRI are often performed to visualise the liver and bile ducts. These tests help rule out other liver conditions and provide a clearer picture of liver health. Liver Biopsy In some cases, a biopsy may be necessary, where a small tissue sample is taken from the liver and examined microscopically. This step is often used to confirm the diagnosis and assess the disease stage, helping guide treatment. What are the treatment options for primary biliary cholangitis? Primary biliary cholangitis treatment aims to slow disease progression, manage symptoms, and improve quality of life. Medication The primary treatment for PBC is ursodeoxycholic acid (UDCA), a bile acid that facilitates better bile flow through the liver and intestines. By reducing the accumulation of toxic bile acids, UDCA can improve liver function, slow disease progression, and decrease the necessity for liver transplantation. It is typically well-tolerated, with minimal side effects. In cases where patients do not respond sufficiently to UDCA, additional medications like obeticholic acid or fibrates may be introduced. These can be utilised in combination with UDCA to enhance treatment efficacy and manage symptoms more effectively. Surgery For patients with end-stage liver disease or severe liver failure resulting from PBC, liver transplantation may be the only viable treatment option. Although transplantation does not cure PBC, as the disease may recur in the new liver, it significantly improves survival rates and enhances the quality of life for patients. This surgical intervention is critical for advanced cases, allowing individuals to regain liver function and enjoy a better overall prognosis. Careful assessment and management by a healthcare team are essential in determining when surgery is appropriate, considering the patient's overall health and the progression of the disease. What is the outlook for primary biliary cholangitis? The outlook for primary biliary cholangitis varies depending on the stage at which it is diagnosed and the individual's response to treatment. Early diagnosis and prompt initiation of UDCA therapy can significantly improve outcomes and slow disease progression. Regular monitoring and management of symptoms and complications are crucial for maintaining quality of life. How long can you live with primary biliary cholangitis? The life expectancy for individuals with PBC has improved significantly with the use of UDCA and advancements in liver transplantation. Many people with PBC can live for over 20 years after diagnosis, especially when the condition is detected and treated early. However, the disease's progression and individual factors can influence life expectancy. How do I take care of ourselves while living with PBC? Living with primary biliary cholangitis requires a proactive approach to manage the condition and maintain overall health. Some key strategies include: Adhering to prescribed medications, such as UDCA Maintaining a healthy diet and exercising regularly Avoiding alcohol and other substances that can harm the liver Attending regular check-ups with your healthcare provider Monitoring for and managing complications, such as osteoporosis or vitamin deficiencies Seeking support from family, friends, or support groups Conclusion Primary biliary cholangitis is a serious, chronic liver disease that requires early detection and proactive management to improve outcomes and quality of life. If you suspect you may have PBC or have been recently diagnosed, consult with your healthcare provider to develop a personalised treatment plan. Metropolis Healthcare, a leading chain of diagnostic labs across India, offers accurate pathology testing and health check-up services to support the early detection and monitoring of PBC. The team of qualified blood collection technicians can perform at-home visits for blood samples, which are processed at Metropolis' advanced diagnostic labs. Test reports are conveniently shared online via email and the user-friendly Metropolis TruHealth app, empowering patients to take control of their health.
Behcet's Disease: A Rare Condition Affecting Multiple Body Systems
What is Behcet's disease? Behcet's disease, also known as Behcet's syndrome, is a chronic inflammatory condition that leads to inflammation of blood vessels and tissues in multiple parts of the body. The inflammation can affect the mouth, eyes, skin, joints, blood vessels, digestive system, and brain. Who gets Behcet's disease? Behcet's disease can affect people of all ages, genders, and ethnicities, but it is more common in certain populations. The condition most often affects young adults in their 20s and 30s, although symptoms can begin earlier or later in life. Behcet's disease is more prevalent in regions along the ancient Silk Road trade route, including Turkey, the Middle East, and parts of Asia. Genetic factors likely play a role, with certain gene variations increasing risk. What are the symptoms of Behcet's disease? Behçet's disease is a complex autoimmune disorder characterised by a variety of symptoms that can vary widely among individuals. The Behçet's disease symptoms often fluctuate in intensity, and many can be painful or debilitating. Here are some of the most common signs and symptoms associated with this condition: Mouth Ulcers: One of the most characteristic Behçet's disease symptoms is the presence of painful, recurring mouth ulcers. These sores, resembling canker sores, can make eating, drinking, and speaking difficult. They may take several weeks to heal and can reappear frequently, causing significant discomfort. Genital Ulcers: Similar to oral ulcers, genital sores are another hallmark of Behçet's disease. These painful lesions can develop on the scrotum, penis, or vulva, and can be particularly distressing, impacting quality of life and sexual health. Eye Inflammation: Uveitis, or inflammation of the eye, is a common complication, affecting over half of those with Behçet's disease. Symptoms may include redness, pain, blurry vision, and sensitivity to light. If not treated promptly, this inflammation can lead to severe complications, including vision loss. Skin Problems: Various skin issues can occur, including acne-like bumps, painful nodules known as erythema nodosum, and other sores or lesions. These skin manifestations can vary in appearance and severity. Joint Pain and Swelling: Approximately half of those with Behçet's disease symptoms experience joint pain and swelling, often affecting the knees, ankles, elbows, and wrists. This arthritis can cause stiffness and discomfort, impacting daily activities. Blood Clots: Behçet's disease causes inflammation within blood vessels, increasing the risk of developing blood clots, such as deep vein thrombosis (DVT) in the legs or cerebral venous sinus thrombosis in the brain, which can pose serious health risks. Digestive Problems: Inflammation along the digestive tract can lead to symptoms such as abdominal pain, diarrhoea, and bleeding. These gastrointestinal issues may mimic those seen in inflammatory bowel diseases. Brain and Nervous System Complications: In severe cases, Behçet's disease can affect the brain and nervous system, potentially leading to conditions such as meningitis, seizures, stroke, and impaired balance or movement. These neurological symptoms highlight the seriousness of the disease and the need for effective management. Behçet's disease is a multifaceted condition that requires ongoing monitoring and treatment by healthcare professionals to manage symptoms effectively and improve patients' quality of life. What causes Behcet's disease? The exact Behcet's disease causes are unknown, but it is believed to arise from a combination of genetic and environmental factors. Individuals with specific gene variations, particularly the HLA-B51 gene, are at a heightened risk for developing the condition. Additionally, abnormal immune system responses likely play a significant role in its onset. Environmental triggers, such as viral or bacterial infections, may provoke these immune reactions, leading to the destructive inflammation characteristic of Behçet's disease in genetically predisposed individuals. This complex interplay between genetics and environmental factors contributes to the variability in symptoms and severity among those affected. Who is at risk of developing Behcet's disease? Several factors may increase the risk of developing Behçet's disease. Genetics plays a significant role, as individuals with a family history or relatives diagnosed with the condition are more susceptible. Ethnicity is another important factor, with higher prevalence among people of Turkish, Middle Eastern, or Asian descent. Age is also a key consideration, as symptoms typically emerge between the ages of 20 and 40. Additionally, environmental factors, such as infections, may contribute to triggering the disease in those with a genetic predisposition. Understanding these risk factors can help in early identification and management of the condition. How is Behcet's disease diagnosed? Diagnosing Behcet's disease can be challenging, as there is no single definitive test. Instead, doctors must rely on a combination of exams, tests and the patient's clinical history. Some common components of a Behcet's disease diagnosis may include: Medical history and physical exam to document symptoms Blood tests to check for signs of inflammation and rule out other conditions Pathergy test to see if the skin is hypersensitive and overreacts to minor injuries Imaging tests like X-rays, CT, or MRI to assess joint, organ, or blood vessel damage Skin or tissue biopsy to examine for signs of inflammation under a microscope Is Behcet's disease hereditary? While Behcet's disease can run in families, suggesting a genetic component, it does not have a straightforward inheritance pattern. Most cases are sporadic, meaning they occur without a known family history. However, having the HLA-B51 gene variation does increase the risk, and genetic factors likely interact with environmental triggers. How is Behcet's disease treated? There is currently no cure for Behcet's disease, so treatment focuses on reducing inflammation, relieving symptoms, and preventing complications. Some common Behcet's disease treatment approaches include: Anti-inflammatory medications to quickly reduce inflammation throughout the body Immunosuppressant drugs to decrease harmful immune system activity Biologic medications to target specific inflammatory processes Antibiotics, antivirals or antifungals to treat infections that may trigger flares Topical therapies and mouth rinses to manage skin and mouth sores Treatment plans are highly individualised based on each person's specific symptoms and disease severity. Working closely with a rheumatologist and other specialists is key for optimal Behcet's disease treatment. What is the outlook for people with Behcet's disease? The course of Behcet's disease is unpredictable, with periods of remission alternating with flare-ups. While the condition is not considered fatal, serious complications like stroke, blindness, or internal bleeding can occur without proper treatment. However, with early diagnosis and a comprehensive treatment plan, most people with Behcet's disease can effectively control symptoms and maintain a good quality of life. Is Behcet's disease fatal? In the vast majority of cases, Behcet's disease is not life-threatening. However, serious complications can arise, such as ruptured blood vessels, stroke, or meningitis. Careful monitoring and treatment adherence are important to reduce risks. What are ways to successfully cope with Behcet's disease? Living with a chronic condition like Behcet's disease can be challenging, both physically and emotionally. Some strategies that may help include: Learning as much as possible about the condition Maintaining open communication with your healthcare team Following your prescribed treatment plan consistently Keeping a symptom journal to identify potential triggers Practising stress management and relaxation techniques Connecting with others through local or online support groups Making lifestyle changes to support overall health, such as eating an anti-inflammatory diet, getting adequate sleep, and exercising regularly as able Conclusion Receiving a Behcet's disease diagnosis can feel overwhelming, but know that you are not alone. With the care of experienced healthcare providers and an individualised treatment plan, it is possible to successfully manage this complex condition. If you are experiencing symptoms that may point to Behcet's disease, consider reaching out to Metropolis Healthcare for expert diagnostic testing services. Their team of qualified blood collection technicians can conveniently come to your home to collect samples, which are then processed in Metropolis' state-of-the-art labs. Timely access to accurate test results can be an important first step on the path to feeling your best. Remember, knowledge is power - and taking a proactive role in your health is always worthwhile.
डायलिसिस: प्रकार, यह कैसे काम करता है, प्रक्रिया और दुष्प्रभाव
डायलिसिस क्या है? डायलिसिस एक चिकित्सा प्रक्रिया है जो उन मरीजों के लिए होती है जो किडनी रोग से ग्रस्त होते हैं, खासकर वे जिनकी किडनी पूरी तरह से काम करना बंद कर देती है। जब किडनी रक्त को ठीक से छानने में सक्षम नहीं होती, तो रक्त में वेस्ट और विषैले पदार्थ जमा होने लगते हैं। ऐसे में, डायलिसिस शरीर में एक कृत्रिम किडनी की तरह काम करती है, जो अतिरिक्त वेस्ट और फ्लूइड्स को शरीर से बाहर निकालने का कार्य करती है। किसे डायलिसिस की ज़रूरत होती है? डायलिसिस केवल उन व्यक्तियों को आवश्यकता होती है जो अत्यधिक गंभीर किडनी रोग, जिसे 'किडनी फेल्योर' कहा जाता है, से प्रभावित होते हैं। विभिन्न चिकित्सीय कारण, जैसे कि क्रॉनिक डायबिटीज, आनुवांशिक कारण, उच्च रक्तचाप, या चोट, किडनी फेल्योर का कारण बन सकते हैं। इन स्थितियों में किडनी इतनी अधिक क्षतिग्रस्त हो जाती है कि व्यक्ति को जीवन के लिए किडनी ट्रांसप्लांट या डायलिसिस की आवश्यकता होती है। डायलिसिस की आवश्यकता मरीज को उन लक्षणों के आधार पर हो सकती है जैसे भ्रम या सांस की कमी, जो किडनी फेल्योर का संकेत देते हैं। चरणों के आधार पर, चिकित्सक किडनी रोग की गंभीरता का निर्धारण कर सकते हैं। यह डायलिसिस उपचार उन लोगों के लिए आवश्यक है जो स्टेज 5 या गंभीर किडनी रोग से पीड़ित होते हैं। डायलिसिस मरीजों की अनुमानित ग्लोमेरुलर फिल्ट्रेशन रेट (eGFRs) काफी कम होती है, जो 15 mL/min से कम होती है और किडनी फंक्शन का संकेत देती है। इसलिए, यदि कोई व्यक्ति क्रॉनिक किडनी डिजीज से पीड़ित है, तो तुरंत किसी हेल्थकेयर प्रोफेशनल से संपर्क करना चाहिए। किडनी क्या करती है? किडनी शरीर का अद्वितीय फिल्टर सिस्टम है। यह आपके शरीर से अतिरिक्त फ्लूइड और वेस्ट को हटाती है और शरीर की कोशिकाओं द्वारा उत्पन्न एसिड को कम करती है, जिससे पानी, नमक, और खनिज स्तरों को बनाए रखने में मदद मिलती है। यह रक्तचाप को नियंत्रित करने में भी मदद करती है। किडनी रक्त से वेस्ट को छानने के दौरान मूत्र का निर्माण करती है। डायलिसिस के प्रकार क्या हैं? डायलिसिस के दो मुख्य प्रकार होते हैं: हेमोडायलिसिस पेरिटोनियल डायलिसिस हेमोडायलिसिस क्या है? हेमोडायलिसिस एक प्रक्रिया है जिसमें एक डायलिसिस मशीन और एक विशेष फिल्टर का उपयोग करके आपके रक्त को साफ किया जाता है। हेमोडायलिसिस आमतौर पर हफ्ते में 3 से 5 बार डायलिसिस सेंटर में किया जाता है। हेमोडायलिसिस का एक्सेस आपके हाथ में होगा। हेमोडायलिसिस में, आपको शुरुआत में एक अस्थायी कैथेटर मिलता है जो नस के माध्यम से आपके दिल की ओर जाता है। इसे 90 दिनों तक उपयोग कर सकते हैं और उसके बाद संक्रमण से बचने के लिए इसे बदलने की आवश्यकता होती है। एक बार जब आपको स्थायी कैथेटर मिल जाता है, तो आप इसे अस्थायी कैथेटर से बदल सकते हैं। हेमोडायलिसिस से पहले क्या होता है? हेमोडायलिसिस शुरू करने से पहले ब्लडस्ट्रीम एक्सेस को सुगम बनाने के लिए आपको एक छोटी सर्जिकल डायलिसिस प्रक्रिया से गुजरना होगा। आपके पास निम्नलिखित हो सकते हैं: एक डायलिसिस सर्जन आपकी बांह में एक आर्टरी और वेन्स को जोड़ता है, जिसे आर्टरीओवेनस फिस्टुला (AV फिस्टुला) कहा जाता है। यदि आर्टरी और वेन्स पर्याप्त बड़ी नहीं होतीं, तो सर्जन एक नरम, खोखली ट्यूब (ग्राफ्ट) का उपयोग करके उन्हें जोड़ता है। आर्टरीओवेनस फिस्टुला (AV फिस्टुला) बनाने की सर्जरी आमतौर पर हेमोडायलिसिस शुरू करने से 4 से 8 हफ्ते पहले की जाती है। यह प्रक्रिया फिस्टुला के आसपास की त्वचा और ऊतकों को ठीक होने में मदद करती है। अधिकांश मरीजों को हर हफ्ते 3-4 घंटे तक हेमोडायलिसिस या डायलिसिस उपचार की आवश्यकता होती है, और इसे आप घर पर या अस्पताल में करवा सकते हैं। अगर तेजी से डायलिसिस करने की ज़रूरत होती है, तो आपका डॉक्टर आपकी गर्दन, पैर या छाती में अस्थायी एक्सेस के लिए एक कैथेटर (पतली ट्यूब) का उपयोग करेगा। हेमोडायलिसिस के दौरान क्या होता है? हेमोडायलिसिस या डायलिसिस उपचार के दौरान रक्त को ट्यूब्स के माध्यम से शरीर से डायलिसिस मशीन में स्थानांतरित किया जाता है। रक्त मशीन में एक डायलाइज़र से गुजरता है, एक फिल्टर जो आपके रक्त से वेस्ट और अतिरिक्त फ्लूइड को निकालता है। इस प्रक्रिया के बाद, डायलिसिस मशीन से साफ हुआ रक्त फिर से ट्यूब्स के माध्यम से आपके शरीर में वापस आ जाता है। इस प्रक्रिया को वैस्कुलर एक्सेस कहा जाता है। हेमोडायलिसिस के बाद क्या होता है? हेमोडायलिसिस या डायलिसिस के बाद, आपको कुछ घंटों के लिए थकान महसूस हो सकती है। हालांकि, जो लोग नियमित हेमोडायलिसिस से अधिक बार डायलिसिस करवाते हैं, वे आमतौर पर बेहतर महसूस करते हैं, अधिक ऊर्जा पाते हैं और उनकी नींद भी बेहतर होती है। पेरिटोनियल डायलिसिस क्या है? यह किडनी फेल्योर के इलाज के लिए एक प्रकार की डायलिसिस है, जिसमें आपके पेट में एक विशेष फ्लूइड डाला जाता है, जो रक्त को साफ करने के लिए शरीर से बाहर निकाला जाता है। एक सर्जरी के द्वारा पेट में एक कैथेटर डाला जाता है, जिसके माध्यम से एक स्टेराइल क्लीनसिंग डायलिसिस फ्लूइड आपके पेट में इंजेक्ट किया जाता है। डायलिसिस प्रक्रिया पूरी होने के बाद, यह फ्लूइड शरीर से बाहर निकाला जाता है, और कैथेटर के माध्यम से शरीर में रहता है। पेरिटोनियल डायलिसिस से पहले क्या होता है? पेरिटोनियल डायलिसिस शुरू करने से लगभग तीन सप्ताह पहले, आपको एक मामूली सर्जिकल प्रक्रिया से गुजरना पड़ता है। इस प्रक्रिया में, डायलिसिस सर्जन आपके पेट में और पेरिटोनियम के भीतर एक पतली और मुलायम ट्यूब, जिसे कैथेटर कहते हैं, डालते हैं। आप इसे घर पर भी कर सकते हैं, और कैथेटर-साइट संक्रमण से बचने के लिए सावधानियां बरत सकते हैं। पेरिटोनियल डायलिसिस के दौरान क्या होता है? पेरिटोनियल डायलिसिस के दौरान: Y-आकार की ट्यूब की एक शाखा कैथेटर से जुड़ी होती है। यह ट्यूब एक डायलिसिस सॉल्यूशन से भरे बैग से जुड़ी होती है। डायलिसिस बैग को खाली करें। इसे खाली करने में आमतौर पर 10 मिनट का समय लगता है। फिर ट्यूब और कैथेटर को डिस्कनेक्ट करें। इसके बाद, कैथेटर का कैप हटा लें। आप अपनी सामान्य गतिविधियों को जारी रख सकते हैं, जबकि पेरिटोनियल कैविटी में इंजेक्ट किए गए सॉल्यूशन से आपका शरीर अतिरिक्त फ्लूइड और वेस्ट को अवशोषित करता है। यह प्रक्रिया लगभग 60-90 मिनट तक चल सकती है। कैथेटर का कवर हटाने के बाद, फ्लूइड को Y-आकार की ट्यूब की विपरीत शाखा से एक ताजे और साफ बैग में डालें। इन सभी चरणों को दिन में चार बार दोहराना होता है। आप पेरिटोनियल डायलिसिस को रात के समय भी कर सकते हैं। इसे ऑटोमेटेड पेरिटोनियल डायलिसिस (APD) कहा जाता है, जिसमें सॉल्यूशन को सोते समय साइकलर पंप्स के माध्यम से आपके शरीर में डाला और बाहर निकाला जाता है। इस प्रक्रिया के दौरान, जैसे ही आप सोते हैं, डायलिसिस सॉल्यूशन पूरी रात आपके पेट में रहता है। पेरिटोनियल डायलिसिस के बाद क्या होता है? हालांकि यह प्रक्रिया कुछ असुविधा पैदा कर सकती है, लेकिन यह दर्दनाक नहीं है। पेरिटोनियल डायलिसिस के बाद, आपको पेट भरे या फूले होने का अहसास हो सकता है। जब आपके पेट में फ्लूइड भरा होता है, तो यह सामान्य से अधिक बाहर निकल सकता है। हेमोडायलिसिस के संभावित जोखिम या जटिलताएं क्या हैं? हेमोडायलिसिस के दौरान आपको हाइपरटेंशन, कार्डियक अरेथमिया, HD मेम्ब्रेन प्रतिक्रिया, एयर एम्बोलिज्म, एलर्जिक प्रतिक्रिया जैसी जटिलताओं का सामना हो सकता है। हालांकि, एयर एम्बोलिज्म और एलर्जिक प्रतिक्रियाओं जैसी जटिलताएं अब उन्नत HD मशीनों के कारण कम हो गई हैं। कुछ संभावित जोखिमों में शामिल हैं: डायलिसिस उपचार के दौरान मशीन से ट्यूब या सुई निकलने का जोखिम हो सकता है। इसके अलावा, हेमोडायलिसिस के दौरान आपके रक्तचाप में गिरावट भी हो सकती है। पेरिटोनियल डायलिसिस के संभावित जोखिम या जटिलताएं क्या हैं? कुछ लोगों में कैथेटर के चारों ओर त्वचा संक्रमण हो सकता है। इसके अलावा, आपको पेरिटोनिटिस हो सकता है, एक बीमारी जो बैक्टीरिया के कारण हो सकती है जो आपके कैथेटर के माध्यम से आपके पेट में प्रवेश कर सकती है। बुखार, उल्टी, मतली, और पेट दर्द अन्य संभावित डायलिसिस साइड इफेक्ट्स हैं। समय के साथ, पेरिटोनियल डायलिसिस के कारण आपके पेट की मांसपेशियां कमजोर हो सकती हैं, खासकर जब पंपिंग फ्लूइड और कैथेटर के दबाव के कारण। यदि पेट की मांसपेशियों के माध्यम से कोई अंग, जैसे कि छोटी आंत, बाहर निकलता है, तो यह हर्निया का कारण बन सकता है। यह उभार आपके ऊपरी जांघ या नाभि के पास दिखाई दे सकता है। हालांकि, एक सर्जन हर्निया का इलाज सर्जिकल तरीके से कर सकता है। इसके अलावा, पेरिटोनियल डायलिसिस के दौरान आपके शरीर में डायलिसिस सॉल्यूशन में मौजूद शुगर (डेक्सट्रोज) का अवशोषण होता है, जिसके कारण वजन में वृद्धि हो सकती है। डायलिसिस पर किसी के लिए दृष्टिकोण (प्रॉग्नोसिस) क्या है? एक डायलिसिस मरीज आसानी से 10-20 साल जीवित रह सकता है। डायलिसिस पर दृष्टिकोण (प्रॉग्नोसिस) किडनी फेल्योर के कारण, उम्र, सामान्य स्वास्थ्य, और अन्य कारकों के अनुसार भिन्न होता है। इसके अलावा, किडनी ट्रांसप्लांट के बाद इस डायलिसिस को बंद किया जा सकता है। क्या डायलिसिस पर रहते हुए मेरी गतिविधियों पर प्रतिबंध रहेगा? कई डायलिसिस मरीज अपनी व्यस्त जिंदगी जारी रखते हैं, काम करते हैं, परिवार बनाते हैं, और यात्रा करते हैं। जब आप यात्रा करते हैं तो कुछ डायलिसिस चार्जेस को प्राप्त करके नए क्षेत्र में डायलिसिस प्राप्त करने के लिए आपके हेल्थकेयर प्रैक्टिशनर आपकी व्यवस्था करने में मदद कर सकते हैं। यदि आवश्यक हो, तो डायलिसिस बैग्स और एक मोबाइल होम डायलिसिस मशीन को किसी भी प्रकार के स्व-डायलिसिस के लिए लाया जा सकता है। जब पेरिटोनियल डायलिसिस सॉल्यूशन पेट में भर जाता है, तो डायलिसिस उपचार ले रहे व्यक्तियों को अपने शारीरिक व्यायाम या अन्य शारीरिक गतिविधियों को सीमित करने की आवश्यकता हो सकती है। इस दौरान, यह सलाह दी जाती है कि आप अपने पेरिटोनियल डायलिसिस प्रोवाइडर से विशेष खेलों या शारीरिक गतिविधियों में भाग लेने के बारे में परामर्श लें। डॉक्टर को कब कॉल करना चाहिए? आपको निम्नलिखित स्थितियों में अपने हेल्थकेयर प्रोवाइडर को कॉल करने पर विचार करना चाहिए: मूत्र त्यागने में समस्या बेहोशी, चक्कर आना, असामान्य प्यास (डिहाइड्रेशन), या अन्य हाइपोटेंशन से संबंधित लक्षण उल्टी और मतली AV फिस्टुला में लालिमा, बुखार, या कैथेटर साइट से बहाव जैसी संक्रमण के लक्षण पेट में असामान्य दर्द ग्रोइन या पेट में उभार निष्कर्ष: डायलिसिस उन मरीजों के लिए जीवनरक्षक उपचार है जो एंड-स्टेज रीनल डिजीज (ESRD) या किडनी फेल्योर से जूझ रहे हैं। यदि आपको लंबे समय तक डायलिसिस की आवश्यकता हो, तो आप इसकी लागत के बारे में जानकारी ले सकते हैं। आपका हेल्थकेयर प्रोवाइडर डायलिसिस के विभिन्न प्रकारों और उपलब्ध विकल्पों पर चर्चा करेगा, जिससे आप यह निर्णय ले सकेंगे कि आप घर पर या डायलिसिस सेंटर में उपचार करवाना चाहेंगे। इसके अतिरिक्त, आपके डॉक्टर आपकी किडनी की कार्यक्षमता का मूल्यांकन करने के लिए रक्त परीक्षण या अन्य आवश्यक परीक्षणों की सलाह दे सकते हैं, और उसके आधार पर डायलिसिस के उपयुक्त विकल्प सुझा सकते हैं। मेट्रोपोलिस लैब्स, एक प्रमुख पैथोलॉजी सेवा प्रदाता, जो घर पर रक्त परीक्षण की सुविधा प्रदान करता है, के साथ आप कुशल पेशेवरों और पैथोलॉजिस्टों से अपनी रिपोर्ट प्राप्त कर सकते हैं।
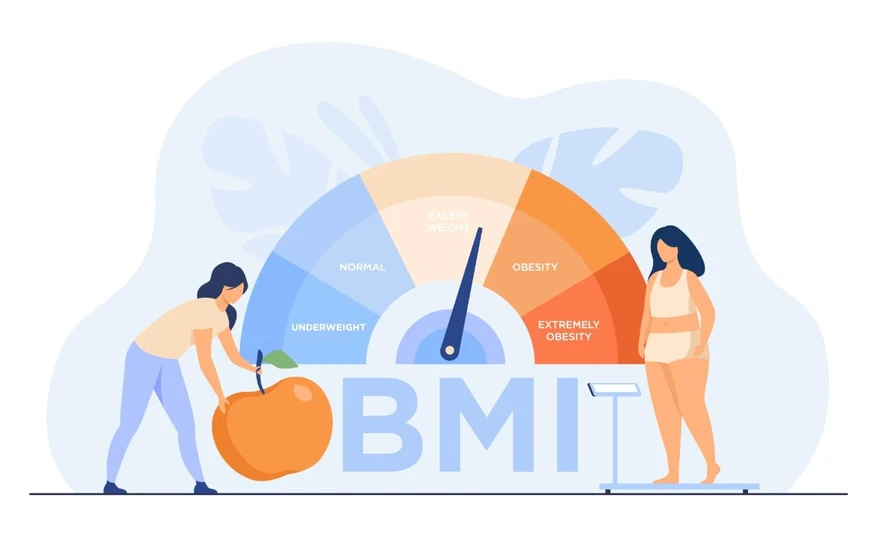
बीएमआई (बॉडी मास इंडेक्स): चार्ट और गणना कैसे करें
बॉडी मास इंडेक्स (BMI) क्या है? स्वास्थ्य जांच या जिम ब्रोशर में आपने शायद बॉडी मास इंडेक्स (BMI) के बारे में सुना होगा। यह एक सरल माप है जिसका उपयोग स्वास्थ्य विशेषज्ञ आपके कद और वजन के अनुपात की जांच करने के लिए करते हैं। इस माप को निकालने का तरीका यह है कि आप अपने वजन (किलोग्राम में) को अपनी ऊंचाई (मीटर में) के वर्ग से विभाजित करते हैं। उदाहरण के लिए, यदि किसी व्यक्ति का वजन 70 किलोग्राम है और उसकी ऊंचाई 1.75 मीटर है, तो उसका BMI इस प्रकार निकाला जाएगा: BMI = 70 / (1.75^2) = 22.9 यह संख्या आपके शरीर में कुल फैट की मात्रा का अनुमान देती है; जितनी अधिक संख्या होगी, आमतौर पर उतनी ही अधिक फैट की मात्रा होगी। BMI का उपयोग किस लिए किया जाता है? स्वास्थ्य विशेषज्ञ BMI का उपयोग प्रारंभिक जांच के रूप में करते हैं। यह विभिन्न वजन श्रेणियों की पहचान करने और कुछ स्वास्थ्य समस्याओं के लिए एक स्क्रीनिंग उपकरण के रूप में काम करता है। BMI (बॉडी मास इंडेक्स) के द्वारा वजन प्रकारों का निदान एक संख्यात्मक माप है, जो व्यक्ति की ऊंचाई और वजन के आधार पर निकाला जाता है। यह माप अक्सर लोगों को उनके BMI मान के अनुसार विभिन्न वजन श्रेणियों में वर्गीकृत करने के लिए उपयोग किया जाता है। सामान्यतः, स्वास्थ्य विशेषज्ञ निम्नलिखित BMI रेंज (kg/m² में) के आधार पर विभिन्न वजन श्रेणियों का निर्धारण करते हैं: अल्पवजन: 18.5 से कम उपयुक्त सीमा: 18.5 से 24.9 अधिक वजन: 25 से 29.9 क्लास I मोटापा: 30 से 34.9 क्लास II मोटापा: 35 से 39.9 क्लास III मोटापा: 40 या उससे अधिक BMI स्वास्थ्य विशेषज्ञों को यह समझने का एक सरल तरीका प्रदान करता है कि कोई व्यक्ति अल्पवजन, सामान्य वजन, अधिक वजन या मोटापे से ग्रस्त है। यह वर्गीकरण वजन से संबंधित समस्याओं का आकलन करने और वजन की स्थिति से जुड़े संभावित स्वास्थ्य जोखिमों का अनुमान लगाने में सहायक होता है। हालांकि, BMI या बॉडी मास इंडेक्स वजन प्रकारों की पहचान के लिए एकमात्र उपकरण नहीं है। अन्य विधियों में कमर की परिधि मापना या शरीर के विशिष्ट क्षेत्रों, जैसे कंधे के ब्लेड के नीचे और ऊपरी बांह की पीठ पर त्वचा की मोटाई मापने के लिए कैलिपर्स का उपयोग करना शामिल है। स्वास्थ्य जोखिमों की स्क्रीनिंग के लिए BMI वजन प्रकारों के निदान से परे, BMI का उपयोग वजन से संबंधित स्वास्थ्य जोखिमों का आकलन करने के लिए एक स्क्रीनिंग टूल के रूप में भी किया जाता है। विभिन्न BMI श्रेणियां विभिन्न स्तरों के स्वास्थ्य जोखिमों के साथ सहसंबंधित होती हैं: अल्पवजन: जिनका BMI 18.5 से कम होता है, उन्हें इन्फर्टिलिटी, कुपोषण, कमजोर प्रतिरक्षा प्रणाली और ऑस्टियोपोरोसिस का खतरा हो सकता है। सामान्य वजन: 18.5 से 24.9 के बीच का स्वस्थ BMI रेंज व्यक्ति को वजन से संबंधित स्वास्थ्य समस्याओं के जोखिम से बचाता है, जो अन्य BMI श्रेणियों की तुलना में कम होता है। अधिक वजन: 25 से 29.9 का BMI उच्च रक्तचाप, टाइप 2 डायबिटीज, हृदय रोग, और कुछ प्रकार के कैंसर जैसी बीमारियों के विकास का जोखिम बढ़ाता है। मोटापा: 30 या इससे अधिक का BMI गंभीर स्वास्थ्य समस्याओं जैसे हृदय रोग, स्ट्रोक, स्लीप एपनिया और जोड़ों की समस्याओं के जोखिम को काफी हद तक बढ़ा देता है। स्वास्थ्य विशेषज्ञ BMI का उपयोग वजन से संबंधित संभावित स्वास्थ्य जोखिमों पर चर्चा करने के लिए एक प्रारंभिक बिंदु के रूप में करते हैं। यह जीवनशैली में बदलाव, जैसे आहार में सुधार और व्यायाम की योजना, पर बातचीत को दिशा प्रदान करता है, जिसका उद्देश्य समग्र स्वास्थ्य को बेहतर बनाना और वजन से संबंधित पुरानी बीमारियों के जोखिम को कम करना होता है। हालांकि BMI एक महत्वपूर्ण स्क्रीनिंग टूल है, लेकिन इसकी कुछ सीमाएं भी हैं। यह शरीर में वसा की मात्रा या उसका फैलाव मापने में सक्षम नहीं है, जो व्यक्ति से व्यक्ति में काफी भिन्न हो सकता है। इसलिए, जिन व्यक्तियों का मांसपेशीय ढांचा मजबूत होता है या जिनकी मांसपेशियों की मात्रा अधिक होती है, उनका BMI अधिक हो सकता है, भले ही उनके शरीर में वसा की अस्वास्थ्यकर मात्रा न हो। साथ ही, यह याद रखना जरूरी है कि कई अन्य कारक, जैसे अनुवांशिकता और जीवनशैली की आदतें, भी इन स्वास्थ्य समस्याओं में योगदान कर सकती हैं, भले ही आपका BMI उच्च न हो। मैं अपना BMI कैसे गणना करूं? अब जब हमने समझ लिया कि BMI का उपयोग किस लिए किया जाता है, तो आइए समझें कि BMI की गणना कैसे करें। अपने BMI (बॉडी मास इंडेक्स) को किलोग्राम में निकालने के लिए, अपने वजन को किलोग्राम में अपनी ऊंचाई के वर्ग से विभाजित करें। सूत्र है BMI = वजन (किग्रा) / ऊंचाई^2 (मीटर^2)। उदाहरण के लिए, यदि आपका वजन 70 किलोग्राम है और आपकी ऊंचाई 1.75 मीटर है, तो गणना इस प्रकार होगी: 70 / (1.75 x 1.75) = 22.86। यह परिणाम आपको BMI चार्ट पर सामान्य वजन श्रेणी (18.5 से 24.9 BMI) में रखता है, जो आपकी ऊंचाई के सापेक्ष आपके वजन की स्थिति का एक सामान्य संकेत प्रदान करता है। स्वस्थ BMI क्या है? विश्व स्वास्थ्य संगठन (WHO) के अनुसार, एक स्वस्थ BMI रेंज 18.5 से 24.9 के बीच होती है। लेकिन याद रखें, यह सिर्फ संख्या के बारे में नहीं है! आपका समग्र स्वास्थ्य कई कारकों पर निर्भर करता है, जैसे अनुवांशिकता, शारीरिक गतिविधि का स्तर, जीवनशैली की आदतें (जैसे धूम्रपान या शराब पीना), और मानसिक स्वास्थ्य की स्थिति। BMI की सीमाएं क्या हैं? हालांकि BMI किसी व्यक्ति के शरीर में फैट की मात्रा का अनुमान लगाने का एक सरल और सुलभ तरीका है, लेकिन इसके कुछ सीमाएं भी हैं। वजन प्रकारों के निदान में BMI के उपयोग की सीमाएं वजन प्रकारों की पहचान में BMI की मुख्य कमी यह है कि यह दुबला शरीर द्रव्यमान (आपके शरीर में फैट को छोड़कर हर चीज का वजन) और फैट द्रव्यमान के बीच अंतर नहीं करता है। जिसका अर्थ है कि मांसपेशियों से भरपूर व्यक्ति का BMI उच्च हो सकता है, क्योंकि यह मांसपेशी द्रव्यमान को फैट के रूप में नहीं मापता, हालांकि उनके शरीर में वसा की मात्रा कम हो सकती है। इसके विपरीत, पुरुषों और महिलाओं के लिए एक ही BMI चार्ट का उपयोग किया जाता है, जबकि महिलाओं में आमतौर पर पुरुषों की तुलना में अधिक शरीर में फैट होता है। इसके अलावा, इस चार्ट में समय के साथ वयस्कों की औसत ऊंचाई में होने वाले बदलाव या विशेष जनसंख्या समूहों, जैसे एथलीट, वृद्ध लोग, गर्भवती महिलाएं या वे लोग जो चिकित्सीय स्थितियों के कारण मांसपेशियों की कमी से पीड़ित होते हैं, का ध्यान नहीं रखा जाता है। स्वास्थ्य स्थितियों की स्क्रीनिंग टूल के रूप में BMI के उपयोग की सीमाएं स्वास्थ्य जोखिम आकलन उपकरण के रूप में BMI का उपयोग करने की भी सीमाएं हैं। यह मापता नहीं है कि शरीर में फैट कहाँ या कैसे वितरित होता है; आपके पेट में अतिरिक्त फैट होना बनाम जांघों में होना आपके स्वास्थ्य को अलग तरह से प्रभावित करता है। स्वास्थ्य जोखिम आकलन उपकरण के रूप में BMI का उपयोग करने की भी कुछ सीमाएं हैं। यह यह नहीं मापता कि शरीर में फैट कहाँ और कैसे फैलता है। उदाहरण के लिए, पेट में अतिरिक्त फैट होने से स्वास्थ्य पर एक अलग असर पड़ सकता है, जबकि जांघों में फैट होने से प्रभाव अलग हो सकता है। BMI और मृत्यु दर के बीच का संबंध अक्सर अन्य महत्वपूर्ण कारकों, जैसे पारिवारिक इतिहास, जीवनकाल, या कैंसर का इतिहास, को नजरअंदाज कर देता है। निष्कर्ष: बॉडी मास इंडेक्स (BMI) को समझना आपके वजन और स्वास्थ्य को बेहतर तरीके से जानने का एक महत्वपूर्ण कदम हो सकता है। यह आपके शरीर में फैट के बारे में सामान्य जानकारी देने वाला एक उपयोगी उपकरण है, लेकिन यह याद रखना ज़रूरी है कि यह केवल एक हिस्सा है। आपके समग्र स्वास्थ्य पर कई कारक असर डालते हैं, जैसे अनुवांशिकता, जीवनशैली, मानसिक स्वास्थ्य और अन्य कई चीजें। अगर आपको अपने BMI के बारे में चिंता है और यह आपके स्वास्थ्य के लिए क्या मायने रखता है, तो स्वास्थ्य विशेषज्ञों से संपर्क करने में हिचकिचाएं नहीं। मेट्रोपोलिस हेल्थकेयर में, हम आपकी स्वास्थ्य यात्रा में आपकी सहायता करने के लिए समर्पित हैं। हमारे उन्नत डायग्नोस्टिक लैब्स और योग्य तकनीशियन जो घर पर सैंपल कलेक्शन के लिए तैयार रहते हैं, आपके स्वास्थ्य को प्राथमिकता देना पहले से कहीं अधिक आसान बना देते हैं!



















 WhatsApp
WhatsApp