Latest Blogs
Lipid Disorders: What Are They And How Can I Treat Them?
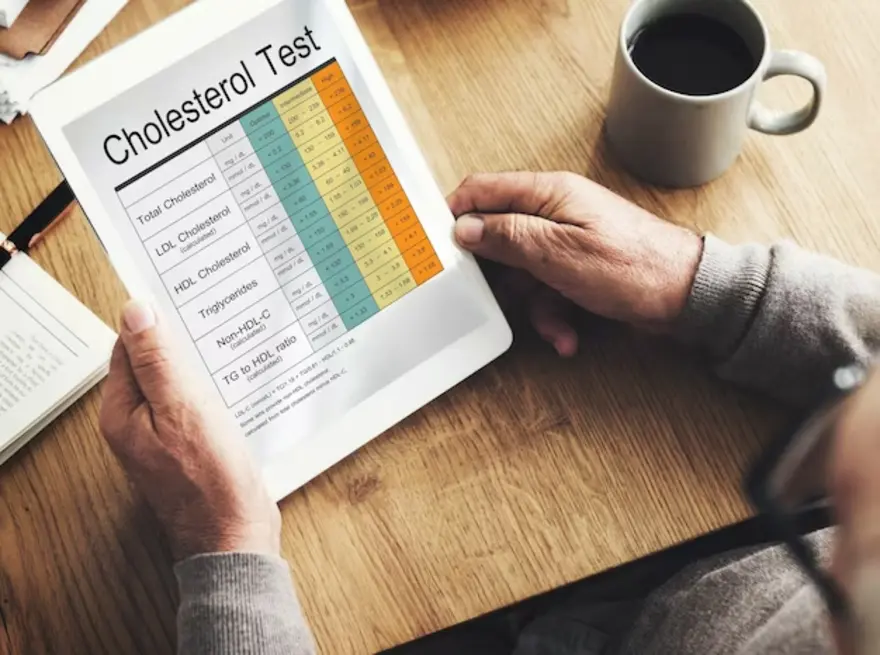
Introduction Do you have a lipid disorder, or are you at risk for one? People with high cholesterol or triglycerides have a lipid disorder. A lipid is a type of fat found in your blood. Lipid disorders are common, but many people don't know they have one. High cholesterol and triglycerides can lead to heart disease, stroke, and other problems. However, you can take steps to lower your risk. This blog will discuss the causes, symptoms, and treatment of lipid disorders. What is a Lipid Disorder? Lipid disorders are conditions that prevent the body from properly metabolising fats. As a result, it can accumulate harmful fats in the blood, increasing the risk for heart disease, stroke, and other serious health problems. However, with proper treatment, many people with lipid disorders can manage their condition and live healthy lives. To the untrained eye, it might seem like all fats are the same. However, there are several different types of fats, each impacting the body differently. You should know the difference between these fats to make informed decisions about your diet and lifestyle. What are The Causes of Lipid Disorder? The causes of lipid disorders vary depending on the type of disorder. In general, however, these conditions are caused by an imbalance in how the body metabolises fats. In addition, it can be due to genetic factors, lifestyle choices, or other underlying health conditions. Some of the most common causes of lipid disorders include: High cholesterol: This is one of the most common causes of lipid disorders. Cholesterol is a type of fat found in the blood. Too much cholesterol can lead to a buildup of plaque in the arteries, which can increase the risk for heart disease, stroke, and other problems. High triglycerides: Triglycerides are another type of fat found in the blood. Like cholesterol, too many triglycerides can lead to plaque buildup in the arteries. It can increase heart disease, stroke, and other problems. Obesity: Obesity is a major risk factor for lipid disorders. People who are obese are more likely to have high cholesterol and triglycerides. Obesity can also lead to other health problems, such as diabetes, which can further increase the risk for lipid disorders. Unhealthy diet: A diet high in saturated and trans fats can increase the risk for lipid disorders. These types of fats can raise cholesterol and triglyceride levels. Lack of exercise: A sedentary lifestyle can also increase the risk for lipid disorders. Exercise helps to improve cholesterol and triglyceride levels. Smoking: Smoking is a major risk factor for lipid disorders. Tobacco smoke contains harmful chemicals that can damage the arteries and raise cholesterol and triglyceride levels. Family history: If you have a family history of lipid disorders, you may be at increased risk for these conditions. Diabetes: Diabetes is a condition that can lead to lipid disorders. People with diabetes are more likely to have high cholesterol and triglycerides. Kidney disease: Kidney disease can also lead to lipid disorders. It is because the kidneys play a role in cholesterol and triglyceride metabolism. What are The Symptoms of Lipid Disorder? Lipid disorder symptoms vary depending on the type of disorder. In general, however, these conditions can cause a variety of problems. Some of the most common symptoms of lipid disorders include: Atherosclerosis is a common complication of lipid disorder. It is when your arteries harden and narrow, and it can lead to a heart attack or stroke. Angina pectoris at rest and exertion (pressing pain, burning sensation in the heart region at rest or during physical work) can also be a symptom of lipid disorders. Other lipid disorder symptoms include sudden dizziness, noise and buzz in the ears, memory impairment, and a sharp decrease in concentration. Some people feel pain in the legs when walking. It can also be a symptom of lipid disorders. Fat deposits are formed in the skin (xanthoma) or the eyelid area (xanthelasma). If you have any of these symptoms, it's important to see your doctor so they can run some tests and determine if you have a lipid disorder. Lipid disorders are often detected by blood tests for lipid screening. This may be a part of Lipid Profile screening , Cardiac Risk Assessment or as part of regular whole body check up. Regular blood glucose level testing for Diabetes mellitus is also recommended as its a precursor for lipid disorders. . Apart from these, some specific tests are also used to detect lipid disorders.These include:: Biochemistry of blood and measuring lipid metabolism will give your doctor an idea of your current state and can start to see the effects of treatment. Determination of the coefficient of atherogenicity - determination of the ratio of high and low-density lipoproteins. Ultrasonic duplex scanning of colour vessels using an ultrasound machine. With its help, the doctor determines the foci of poor circulation and compares the blood flow in paired organs. Magnetic resonance angiography - allows you to evaluate the anatomical and functional features of blood flow. Computed angiography is used to visualise large blood vessels and identify their pathological changes. Treatment for Lipid Disorder With lifestyle changes, medications, and regular screening one can often manage the lipid disorders. Conclusion Not all tests and methods are required. They are prescribed at the doctor's discretion and in the absence of contraindications. The treatment of lipid disorders aims to reduce the risk of atherosclerosis and its complications. To do this, you need to normalise your lifestyle and take medications. For example, it would help if you quit smoking, lead an active lifestyle, and eat right. In addition to diet and physical activity, you need to take drugs that lower cholesterol. These include statins, fibrates, niacin, and other drugs. The choice of drug and dosage is determined by the doctor individually.
Rheumatoid Arthritis Self-Care - Tips for Diagnosis & Managing the Disease
Rheumatoid Arthritis is a chronic disease of the immune system. It is an autoimmune disease where your body’s immune cells attack the lining of the joints, known as synovium. The causes for this condition are attributed to genetic factors and environmental triggers. An inflammatory process characterises Rheumatoid Arthritis in the synovium throughout your body. Your immune system is designed to fight bacteria and other foreign invaders that may cause harm to your body. In Rheumatoid Arthritis, the immune system mistakes the cells of the synovium as a foreign invader and begins attacking this lining of the joints. The synovium produces a fluid that helps the joint move smoothly. But as the cells of the immune system attack it, there is inflammation in these cells, leading to the eventual destruction of the cartilage and bone elements of the joint. As a result, one can experience pain, stiffness, and weakness, among other symptoms. The duration of these symptoms varies from one person to another. For some, the symptoms may be aggressive and progress rapidly. For others, it may take several years. There might also be instances where patients experience a period of time with symptoms (flare) and some with no symptoms (regression). What are The Symptoms of Rheumatoid Arthritis? The intensity of symptoms experienced varies over the different stages of Rheumatoid Arthritis. In the early stages, the symptoms include, Joint stiffness lasts for extended periods, such as half an hour. Experience stiffness in the same joints on both sides of the body. Unexplained pain, swelling and tenderness in smaller joints or multiple joints simultaneously. Fatigue and weakness. Symptoms and discomfort that last longer than six weeks. How is Rheumatoid Arthritis Diagnosed? In the earlier stages, the symptoms of Rheumatoid Arthritis may be similar to other types of arthritis. No singular, gold standard test determines the diagnosis of Rheumatoid Arthritis. Hence, the examination for diagnosing consists of a combination of physical and blood tests. ● Physical Examination The doctor or physician checks the joints for swelling or tenderness. The range of motion is also checked across different joints. During the physical examination, you may be asked about symptoms and your medical and family history for any genetic influences and instances of Rheumatoid Arthritis in relatives. ● Blood Examination Post the physical examination, blood tests are conducted to identify any forms of inflammation and autoantibodies that may indicate Rheumatoid Arthritis. The blood tests may include, Rheumatoid factor (RF) test and CCP antibody test (anti-cyclic citrullinated peptide)–. You can take a CCP Antibody test to distinguish it from other types of Arthritis. CCP antibody test is more specific and has less false positives in comparison to RF Erythrocyte sedimentation rate and C reactive protein – higher levels of these tests may indicate the condition. These are non-specific markers of inflammation Antinuclear antibodies – a positive or negative test helps with diagnosis. Complete blood count (CBC) -- is recommended when the doctor finds low red blood cells, an indicator of Rheumatoid Arthritis. ● Imaging Tests In combination with blood tests, imaging tests reveal the diagnosis and progression of the disease such that the doctor can monitor and provide treatment accordingly. The imaging tests recommended include, X-rays showcase the amount of joint damage. Ultrasound and Magnetic Resonance Imaging (MRI) to provide more details on the condition of the joints. These tests can show if the ends of the bones are slowly eroding over time due to inflammation. Imaging tests are also used between treatments to check the progress and results of medications and treatment. How is Rheumatoid Arthritis treated? There is no specific cure for the disease, but early investigations, diagnosis and medications can help keep symptoms under control. The inflammation can be reduced or stopped, and doctors can prescribe medications to relieve symptoms' remission. Treatment in Rheumatoid Arthritis usually involves medication such as disease-modifying anti-rheumatic drugs. Steroids -- Corticosteroids such as Prednisone help reduce inflammation and pain and slow joint damage. Conventional DMARDs -- are intended to slow the progression of rheumatoid arthritis and save the joints from permanent damage. They are used along with biologic response modifiers, such as methotrexate. Targeted synthetic DMARDs -- these are used when conventional and biological response modifiers do not work. Over-the-counter NSAIDs -- Non-steroidal Anti-Inflammatory Drugs can relieve pain and reduce inflammation during treatment. Therapy The doctor may refer you to a physical or occupational therapist to engage in exercises that can help keep the joint flexible. These modifications are also suggested to one’s daily activities to make them more manageable. For instance, helpful equipment and assistive devices can help you get dressed, get a better grip on holding objects, and so on. Surgery Surgery is often the last resort for rheumatoid arthritis when the medications fail to prevent or slow joint damage. The types of surgery that can reduce pain and improve function include, Tendon repair -- targeted to repair the tendons around the joint that have been loosened or ruptured due to inflammation. Total joint replacement -- the damaged parts of the joints are replaced by prosthetic parts. Synovectomy -- aimed to remove the synovium, the inflamed lining of the joints, to reduce pain and improve flexibility. Joint fusion -- only in cases where replacement is impossible, joint fusion is conducted to relieve pain and stabilise or realign a joint. Discussing the pros and cons of surgery before undertaking the procedure is crucial. Ensure that you are informed of all procedures before and after surgery. Other Forms of Self-Care to Manage Rheumatoid Arthritis While medications and treatment are essential, you can also contribute to your recovery by managing diet and lifestyle choices to control rheumatoid arthritis. Eating healthier, being involved in daily movement such as light walking, proper rest, and using heat treatments to relieve joint pain can help. A diet with Rheumatoid Arthritis may include supplements such as omega-3 fish oil and eliminating habits such as smoking, intake of junk food, and so on. Such habits can contribute to preventing and reversing the effects of rheumatoid arthritis in the long run. Consulting the doctor and therapists on recovery methods and cultivating a positive support system and environment are complementary in the recovery process from Rheumatoid arthritis.
Tips on how to prevent heart disease
1. Go for a heart-healthy diet Experts have concluded that people who follow the right food habits have more than 30% lower risk of heart disease. What is the most-recommended heart-healthy diet? Taking a low-calorie but nutrient-rich food is important. Avoid foods like cakes, biscuits, sausages, pudding, butter, red meat, cheese, fatty dairy products, pasta, bacon, etc. These have high saturated content. Include plenty of fruits, vegetables, whole grains, fish, low-fat dairy products, and nuts in your diet. Include low-fat proteins like yogurt, legumes, skinned poultry, and soy products. Reduce the intake of salt. Limit or avoid canned soups, ketchup, mayonnaise, tomato sauce, soy sauce, etc. How much you eat is as important as what you eat. So, control the portion size of the food you eat. Based on the above recommendations, plan daily menus to make sure that you have a well-balanced diet. 2. Exercise regularly Exercising regularly is one of the major steps to avoid heart attack and keep your heart healthy. It is recommended to be physically active to avoid heart ailments.There are three types of exercises that are very effective in preventing cardiac conditions:. Aerobic exercises like running, cycling, brisk walking, swimming, and skipping help to increase the blood circulation. Exercising also helps to lower the blood pressure and decreases the risk of type 2 diabetes. Resistance training like dumbbells, pushups, resistance bands,, and other such exercises help reduce the LDL also known as “bad cholesterol”. It also reduces body fat, one of the major culprits of heart disease. Body-stretching exercises like yoga and Tai-Chi not only lay a good muscular and skeletal foundation, but also help to reduce stress and anxiety. Although these three physical activities are highly recommended, you can do any physical activity that you like. It could be dancing, jogging or playing a favourite sport like tennis and football. Regular physical activity will surely reduce the chances of heart disease. They are the best tools for cardiovascular disease prevention. 3. Live a tobacco-free life Tobacco control is one of the key elements in preventing heart disease. This is because tobacco increases the risk of heart attack by Damaging lungs Clogging arteries Increasing blood clots, Weakening your immunity Increasing inflammation Moreover, carbon monoxide that enters your bloodstream decreases the oxygen supply to all organs and tissues. It also narrows the blood vessels and increases the blood pressure and heart rate. As a result, your heart is forced to pump blood faster than usual. What happens when you quit smoking? Research has proven that your blood pressure decreases in a day, and blood circulation improves in a couple of weeks after you stop smoking. In a few months, your cough will disappear. In a year, the risk of heart disease reduces by 50%. Live a tobacco-free life to keep your heart healthy. 4. Limit alcohol consumption Several studies have shown that people who took less than two drinks daily had a 20% less risk of heart disease. Heavy drinking can increase the risk of: Elevated Blood pressure Irregular heart rhythm Obesity A disorder in the heart muscle called cardiomyopathy Heart failure Moderate drinking (two drinks for men and one for women) will decrease the risk of heart disease. Limit consumption of alcohol to lower the risk of heart disease. 5. Reduce stress Stress leads to the release of a hormone called cortisol. Cortisol can increase the blood sugar, blood pressure, triglycerides, inflammation, bad cholesterol, and decrease the blood flow to the heart muscles. All these are common risk factors that trigger heart diseases. So you should reduce stress by: Exercising regularly Following relaxing strategies like yoga and meditation Having a hobby that can relax you Being positive Spending time with family and friends Enjoy a stress-free life as it is a precaution against a heart attack. 6. Keep your blood pressure under control Excessive blood pressure narrows the arteries supplying blood to the heart due to the build-up of cholesterol and fat. The hardening of arteries leads to the formation of blood clots. This results in an interruption in the flow of oxygen and nutrients to the heart muscles, and ultimately causes a heart attack. So, it is important to keep your blood pressure under control. To control blood pressure, you have to Sleep well Avoid stress Be physically active Reduce sodium intake and Drink less alcohol. 7. Keep diabetes under control How does diabetes increase the risk of heart disease? It damages the cardiovascular nerves and blood vessels. High sugar levels can also damage your arterial walls. The risk of formation of plaque in the blood vessels is high. It can also increase triglycerides. In cases of known diabetics, it is recommended to get the blood glucose (fasting and postprandial) as well as the HbA1c levels tested at periodic intervals. It is also recommended to test the cholesterol and triglyceride levels regularly as they are closely linked with diabetes. How to keep diabetes under control? Be active. Follow the right meal plan. Check blood sugar levels as directed by the physician. Take the prescribed medications. People in the prediabetes range are also at risk for heart diseases. Hence, they should also follow the necessary precautions. It is recommended to monitor the HbA1c levels and lipid profiles at least annually. 8. Keep your triglycerides and cholesterol under control Cholesterol can be in the form of HDL or LDL. HDL or High-Density Cholesterol is known as good cholesterol. LDL, or Low-Density Cholesterol, similarly is synonymous with bad cholesterol. HDL takes the cholesterol to the liver for disposal. On the other hand, too much LDL may cling to your arteries and block them. Clogged arteries prevent blood from reaching the heart and cause a heart attack. Hence, HDL levels should be high, and LDL should be low, if you want to avoid the risk of heart disease. To raise HDL and lower LDL, you should: Boil, grill, or bake foods instead of deep-frying. Use vegetable oils instead of butter. Consume more citrus fruits, grapes, nuts like almonds, and berries. Include whole grains, beans, lentils, and fish, like sardines and salmon, in your diet. Avoid high-calorie foods. Remove the skin from poultry before cooking. As a precaution against heart attack, you should go for periodic checkups and take the tests recommended by the doctor. One of the most important tests is the HDL test. This helps to find out the risk of developing heart disease. If you have any doubts, take the HDL test as early as possible without any delays. Even individuals with diabetes and also those in the prediabetes range should get regular check ups of the cholesterol and triglyceride levels to prevent the risk of heart diseases. Those with a family history of diabetes and hypertension should go periodically for cardiac risk profile assessment to monitor cardiac health.
Triglycerides: Everything You Need to Know
What are triglycerides? Triglycerides are essential fats you can get from foods like butter, oil, and meat. Most of our body fat are triglycerides because they are unused calories we eat but don’t need. Triglycerides in the blood help transfer adipose fat from one tissue to another and glucose in the blood from the liver. It is also a vital constituent of our skin oils. Eating excess food or food that is high in fat content that the body does not require are instantly stored in the fat cells in the form of triglycerides. The VLDL cholesterol particles in our body help transport Triglycerides to the tissues. The enzyme lipase causes the breakdown of triglycerides into fatty acids and monoglycerides. Chemical composition of triglycerides Triglyceride is chemically an ester formed by bonding three fatty acids and a glycerol molecule. We can broadly classify triglycerides into three main types - saturated, monounsaturated and polyunsaturated fatty acids. Some examples of saturated fats are Butyric acid, lauric acid, palmitic acid, myristic acid and stearic acid. We get them from meats like beef, pork, lamb, and chicken with skin; dairy products like cream, cheese, butter and eggs; and coconut, palm and their products. Saturated fats carry the potential to increase your risk of heart diseases. Therefore, we should limit their consumption in our daily diet. As per AHA (American Heart Association) recommendation, the maximum allowed dietary intake of saturated fats should not be more than 13 g per day (for a daily diet of 1200 calories). It is advisable to replace saturated fats with healthier fats, to eat lean meat and poultry without skin, and substitute your diet with more whole grains, plant proteins, and fruits and vegetables. In comparison, unsaturated fats are healthier for you. Contrary to popular belief, they are now found to help lower your risk of heart disease. Some unsaturated triglycerides are Oleic acid, Sappenic acid, Vaccenic acid, Linoleic acid, Gadoleic acid, and Gondoic acid. Unsaturated triglycerides can be found in avocados, olives, peanuts, canola oil, almonds, hazelnuts, pecans, pumpkins, and sesame seeds. How are triglycerides Different from Cholesterol? Triglycerides and cholesterol are different fats that circulate in our bodies. Triglycerides help store and use the fats, which can later be converted into energy when the body requires it. Cholesterol is essential for building cells, body tissues, and hormones like testosterone and oestrogen. What happens when you have hypertriglyceridemia? Triglyceride levels within the normal range are essential to maintain good health. But high triglyceride levels can cause heart problems like coronary artery disease, heart attacks, and arteriosclerosis (hardening of arterial walls). Very high levels of triglycerides in the body can also cause inflammation of the pancreas, known as pancreatitis. Hypertriglyceridemia is caused by a regular intake of excess calories that the body cannot utilise instantly. This can happen due to Excess sugar intake Obesity Smoking Excess alcohol consumption Consuming certain types of medications like beta blockers, diuretics, steroids, retinoids etc. Genetic disorders Thyroid problems Uncontrolled type 2 diabetes., Liver diseases Kidney diseases Checking your triglycerides level A couple of blood tests known as the lipid profile are prescribed to measure your triglycerides and cholesterol levels that can help you keep tabs on your fat levels. The value of triglyceride level also works as an aid for your physician to help you have a controlled diet in case of a risk of heart disease. Triglycerides are measured as milligrams per decilitre of blood. It is a simple blood test which may require you to fast for 12 hours to get an accurate reading. Interpretation Triglycerides level Normal less than 150mg/dL Borderline high 150-199mg/dL High 200-499mg/dL Very high 500+ mg/dL (Readings are for a normal adult blood sample) It is either done as an individual test or in conjunction with other cholesterol and lipid tests as part of Lipid profile tests. What do the values suggest? Any value over 150mg/dL of triglycerides in the blood can be interpreted as follows: It can increase your risk of heart disease like a stroke. You will also need to test for metabolic disorders (high blood pressure and uncontrolled diabetes and obesity combined). It is an indicator of borderline or type II diabetes. Hypothyroidism Genetic disorders may cause poor conversion of fat into energy. In most cases other cholesterol tests like HDL, LDL , Lipid profile, cardiac profile etc are also done along with triglyceride tests to infer better results. Available treatments for increased triglycerides You should talk to your primary health care physician to make lifestyle changes if triglycerides are above the prescribed range. The following lifestyle changes could be recommended: Weight control Regular physical exercises and activities (for at least 30 mins) Stop smoking Prohibit the use of Alcohol Limit sugar Limit refined and processed foods Using healthy fats instead of saturated fats Intermittent fasting Modified diet to suit your needs and health If lifestyle changes are not enough, your physician may prescribe medications like fish oil, niacin or statins, which may help reduce cholesterol and triglyceride levels. How can you change your diet if you have high triglycerides? If you find that you have hypertriglyceridemia, then there are several options to make your diet more health friendly - Limit the use of starchy vegetables like corn and peas. Canned beans should be replaced with black beans, and you should avoid cooking them with pork or sugar. Too much natural sugar should also be avoided. For example, 2 to 3 servings of fruits should be the limit for a single day. Dried foods for consumption should be measured using a teaspoon. Buy canned fish preserved in water rather than in oil. Coconut is a common ingredient in most of our foods. If you have high triglycerides levels, it is better to talk to a doctor about how much coconut you should consume in your daily diet. Monitor your pasta, white bread, cereals, potatoes, and oatmeal servings. Sugary drinks like soda, fruit juices, iced tea, and sweet coffee should be limited. Bakery items made in butter can be skipped or taken as a tiny serving. Processed meats like bacon, sausage, and hams should be limited or avoided. You can replace butter with canola, olive, walnut or flaxseed oils for cooking and salad dressings. Conclusion Triglyceride levels could be high in your blood without any obvious symptoms or visible signs. High levels of triglycerides are a problem because it causes long-term damage and increases the chances of grave diseases or proves to be fatal. Hence, it is important to keep a regular check on your triglyceride levels and get routine screening done with the Lipid Profile Test. This test covers not just triglycerides but also other cholesterol levels that can cause damage to your body and heart. The frequency of the test is dependent on age and current medical conditions as recommended by your treating physician. At times, certain other blood tests to assess the levels of cardiac markers are also suggested. High triglycerides if left untreated may also contribute towards high blood glucose levels. Hence, it is also recommended to keep a check on the blood glucose levels with regular testing and HbA1c monitoring.
Bone Marrow: Know Functions of Bone Marrow, Histology & Types
Bone marrow is the largest organ in the human body, accounting for almost 5% of the human body weight. It is responsible for the formation of the blood's cellular components. It appears like soft and spongy tissue. The safety and toxicity assessment of the blood-related disorders can be done by studying the bone marrow. Hence a chemical or a toxin causing harm to the bone marrow can be detected by the histology changes in the bone marrow. You can get to know every aspect of bone marrow histology, different types of bone marrow, and the important features of the bone marrow in this article. Where is the Bone Marrow Located? The bones in your body are anatomically made up of 3 parts: compact, spongy, and marrow. The compact bone represents the outer layer of bone and is comparatively stronger. The spongy part forms the end parts of the bone. The bone marrow forms the centre portion of the compact bones and is present at the end parts of spongy bones. The bone marrow is most commonly located in the cavities of long and axial bones; thus, it fills up the cavity of bone and blood vessels. Bone marrow is not rigid like bone. It is jelly-like and fills the cavities left by the trabecular network. What are the Functions of Bone Marrow? The two main functions of the bone marrow are as follows: To produce the blood cells like red blood cells (RBCs or erythrocytes), platelets, and white blood cells (WBCs, namely lymphocytes, granulocytes, and monocytes). This is highly vascular and constitutes Red Bone Marrow. To store the fat. It has adipocytes (fat cells) and constitutes Yellow Bone Marrow. It is comparatively less vascular than red bone marrow. What are the Histological Characteristics of the Bone Marrow? In order to diagnose an abnormal finding, it is necessary to understand the normal make-up of the tissues and cells (histology) that constitute the bone marrow. You, therefore, need to know the normal bone marrow histology. It shows the following characteristics: The exterior of the bone shows the presence of cartilage tissue and tendons. The interior hematopoietic tissue islands and adipose cells are surrounded by vascular sinuses and held within a meshwork of trabecular bone. The outer surface of this meshwork has cells known as osteoblasts. Occasional multinucleated osteoclasts are also present at the trabecular margins. Arterioles and venules occupy the interspaces between the meshwork. Bone marrow stroma consists of a heterogeneous mixture of adipocytes, fibroblasts, macrophage-like cells, and a complex extracellular matrix. Normal histology biopsy specimens show 40-60% non-bony tissue composed of hematopoietic cells. Cellularity will change depending on age. Granulocytes and monocytes are distributed in the specimens, while mature megakaryocytes are easily seen due to their large volumes. A normal bone marrow histology also shows the presence of lymphocytes, mast cells, and plasma cells. What are the Different Types of Bone Marrow? There are two types of bone marrow - red and yellow. Red bone marrow consists of hematopoietic stem cells that produce the components of your whole blood: RBCs, WBCs, and platelets. Yellow bone marrow is responsible for storing fat. It hosts adipocytes and mesenchymal stem cells. These cells preserve fat used in energy production and help develop bones, cartilage, muscles, and fat cells. Fact: Your red bone marrow makes up the entire bone marrow almost until age 7. As you grow gradually, it is replaced by the yellow bone marrow. What are the Key Features of the Bone Marrow that Make it an Important Organ? Here are some key features of the bone marrow: The bone marrow is an important part of your body as it daily produces the whole blood components without which your survival is not possible. The RBCs produced by the bone marrow provide oxygen to the whole body. The WBCs prevent and fight infections while the platelets control bleeding. It also stores fat that helps in the production of energy. Any dysfunction or abnormality in your bone marrow can be dangerous and even fatal. The common symptoms you may experience if your bone marrow is not properly functioning include - Anaemia Frequent bruising Bleeding Frequent infections Tiredness Muscle weakness What are the Diseases of Bone Marrow? Leukaemia is a blood cancer. The bone marrow makes abnormal WBCs. Lymphoma is a cancer of the lymphatic system, and bone marrow may get involved. Aplastic anemia is a condition in which RBCs are not formed in the bone marrow. How is the Abnormality in Bone Marrow Detected? The cells present in the bone marrow, its architecture, and the other features of the bone marrow can be detected by performing some tests. These include - Biopsy: Removal of a small portion of the bone marrow using a needle Aspiration: Removal of the bone marrow concentrate using aspiration Histology and cell assessment: Further detection of an abnormality A bone marrow test is hematopathology testing, which involves identifying cancerous changes in blood and bone marrow. It requires blood smears, bone marrow smears, and histopathology of tissue sections. Based on the clinical features and the condition the clinician may prescribe bone marrow tests from the list of various bone marrow profiles. Can Bone Marrow be Replaced? Bone marrow is the foundation of your blood cells, bones, and muscles. Maintain a healthy bone marrow with adequate proteins and vitamins in your diet. In certain cancers (leukaemia, lymphoma) that originate due to bone marrow abnormality, bone marrow stem cells from a healthy donor are transplanted into the bloodstream of the patient so that they can produce whole blood components.
How to get Enough Calcium to Support Bone and Dental Health?
Calcium is one of the most significant minerals for your body. While calcium is needed for various body processes, it is pivotal to maintain healthy teeth and bones. Almost all calcium in the body is stored in bones and teeth. Bones form the backbone for your musculo-skeletal system, and without teeth, you will not be able to relish your favorite cuisines or win hearts with that cheerful smile. What else do you need calcium for? The body requires calcium for your muscles to move and for nerves to carry messages to and fro between your brain and other body parts. Not just this, blood vessels move blood throughout your body with the help of calcium. It also plays a role in the release of certain hormones that impact many functions in your body. Sure you have enough calcium reserves? Book a test and know for yourself. Calcium for bone and dental health Not getting enough calcium has been linked with reduced bone mass and increased risk of bone fracture. The outermost surface of the tooth, called the tooth enamel, is majorly made up of calcium phosphate molecules called hydroxyapatite. It is the hardest tissue in the body- even harder than the bone. It protects your teeth against erosion, decay and grinding pressures. How does the body maintain blood calcium levels? Calcium circulation in the blood is stringently regulated at any given time. Your body maintains the equilibrium by an efficient interplay of calcium absorbed (through the intestines), calcium mobilized (into and out of the bones and teeth), and calcium excreted (through the kidneys into the urine). If the level of calcium in your blood drops, a gland called parathyroid glands releases a hormone called PTH (parathyroid hormone) into the blood. PTH has calcium regulating properties. It signals cells in bone to release calcium from the bone surfaces. It also triggers the kidney to reclaim more calcium before it is taken out in the urine. All of these make up for the lack of calcium in the blood. However, think of a situation where your body is dealing with a lack of calcium continuously, this may cause release of excessive calcium from your bones and teeth. Eventually, weakening your bones and teeth. How can I get enough calcium naturally? Your body cannot produce calcium. It needs to be taken through natural sources or calcium supplements. Here is a quick list of natural sources of calcium: Curd, Yogurt Milk Sardines and salmon Cheese Tofu Green leafy vegetables, such as broccoli, spinach, turnip leaves Nuts and seeds, especially almonds, sesame, and chia Legumes and grains Fortified alternatives like fortified soy milk, fortified fruit juices, etc. You should aim to get most of your daily nutrient intake from food and beverages, according to the health experts. These foods not only give you calcium but also contain vitamins, other minerals, and abundance of fiber that benefit health. However, if it is difficult to meet daily calcium demands through food, opt for fortified foods and calcium supplements What happens if I don’t get enough calcium? Lack of calcium can result into various bone and teeth related conditions like- Osteoporosis: A condition that causes weak, fragile bones and increases the risk of falling Rickets: A disease in children that results into softer, weaker bones Osteomalacia: The bone softening disease in adults is called osteomalacia. Who can be at risk of having low calcium? Anyone not getting enough calcium through diet can develop calcium deficiency. However, some specific group of people are more likely than others to have enough calcium levels, including: Women after menopause: The body absorbs and retains less calcium after menopause (permanent cessation of periods in women that occurs with age). This makes the bones fragile. People who don’t drink milk or eat other dairy products: Dairy products such as milk, paneer, curd are rich sources of calcium. However, people who are intolerant to lactose (milk sugar), have allergies to milk, or choose a vegan diet lose on the rich calcium source. They must look out for other sources of calcium like lactose-free dairy products, canned fish with bones, certain green leafy vegetables or calcium supplements as suggested by your doctor. Who should consider calcium supplements? If you have got your full body check up or calcium test done and found yourself deficient in calcium, it is pivotal to increase calcium intake and seek expert guidance if you need supplements. At large, calcium supplements may be needed by people who follow a vegan diet, do not have enough dairy products, are getting long-term treatment with corticosteroids, and have certain digestive conditions that disrupt calcium absorption. Calcium supplements are available in many forms and combinations like calcium citrate, calcium carbonate, and along with vitamin D and other minerals. Talk with your doctor or dietitian about which calcium supplement is right for you. A few people may experience gastric upset with supplements. Take your dose with food to reduce the occurrence or intensity of any side effects.
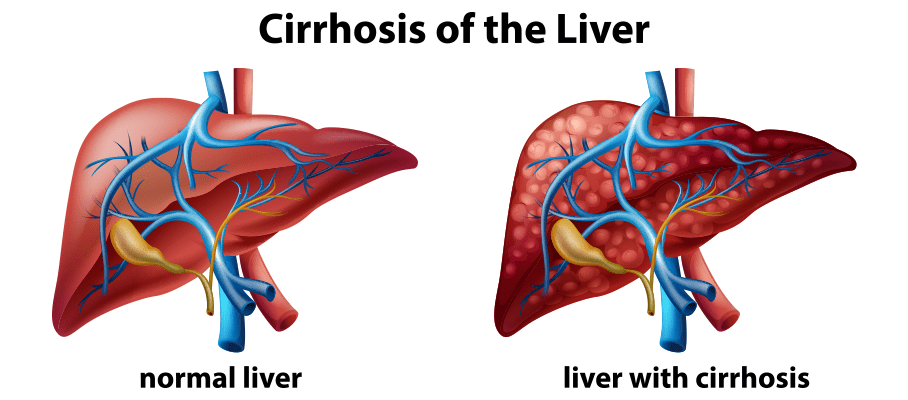
Liver Cirrhosis: Symptoms, Tests and Treatment
Liver is one of the major abdominal organs in humans performing the important function of metabolism of carbohydrates, proteins and fats along with detoxification of harmful substances and toxins from the body by production of bile. It also functions as a major site for production of proteins and clotting factors. It also serves to store glycogen reserves for the body as well as storage of important vitamins and minerals. Keep an eye on your liver health with a liver function test. Here, we have discussed late-stage liver disease called liver cirrhosis, a condition in which the normal architecture of the liver is replaced by fibrotic tissue. Usually after cirrhosis sets in, it is irreversible. As the normal functions of liver are hampered due to fibrosis in liver over time, multiple complications arise, and the most important and troublesome of it is portal hypertension, where blood coming from portal vein (draining blood from entire GIT) toward liver faces excessive resistance due to fibrosis in the liver. Clinically patients with portal hypertension are identified by presence of low blood platelet count and enlarged spleen. Symptoms of Liver Cirrhosis The clinical signs and symptoms in cirrhosis mimic the level of fibrosis in the liver. The early signs usually include feeling tired or weak, loss of appetite, unintentionally losing weight, nausea, vomiting, mild pain or discomfort in the abdomen. Other features associated with loss of normal liver functions are development of jaundice coagulation disorder, encephalopathy, etc. While any liver insult can ultimately lead on to cirrhosis unless intervened in time, the most common causes are chronic alcohol use, chronic viral infections affecting liver like hepatitis B and C viruses, biliary cirrhosis, autoimmune liver inflammation and rarely some inherited liver disorders. Overall chronic alcohol consumption remains to be a major cause for cirrhosis in India and worldwide. The accurate diagnosis of alcohol causing liver cirrhosis requires accurate history regarding the amount and duration of intake along with corroborative symptoms like vague upper abdominal pain, nausea, vomiting, diarrhoea and even malaise. Meanwhile a few patients may present straight away with complications of cirrhosis like abdominal distension, edema and even gastrointestinal variceal haemorrhage. Test for Liver Cirrhosis Laboratory investigations may reveal signs of acute blood loss as in anemia along with nutritional deficiency with low platelet counts commonly. Liver function tests may show signs of mild increase in serum bilirubin as fibrosis in liver hampers its elimination along with elevation in levels of liver enzymes in blood, both ALT and AST are elevated but AST levels higher than ALT approximately in a ratio of 2:1 are typical of alcoholic liver disease and cirrhosis. Coagulation profile may show increased PT time. Pathological confirmation of cirrhosis can be obtained with the help of liver biopsy. For patients with suspected viral cause for cirrhosis blood tests may be done for detecting HCV RNA, HBsAg, HBeAg and Anti HBe levels along with quantitative HBV DNA levels. For autoimmune causes of cirrhosis, blood levels of antinuclear antibody (ANA) or anti-smooth-muscle antibody (ASMA) may be done. Anti-Mitochondrial auto-antibodies (AMA) are present in patients developing cirrhosis due to biliary cause along with other signs of cholestasis. Fibroscan may help detect the level of fibrosis in the liver and the need for liver transplant in future. For patients who have risk factors associated with development of cirrhosis it is prudent to rule out development of portal hypertension at the earliest. One should be vigilant for development of ascites and features of hypersplenism like low platelet counts (thrombocytopenia) and low WBC counts (leukopenia). It is important to rule out variceal bleeding in suspected patients at onset of cirrhosis with the help of endoscopy. Ascitic fluid study may be done to rule out other causes for it. Apart from these radiological investigations like CT scan or MRI abdomen should be done to evaluate the level of cirrhosis and portal hypertension. Treatment for Liver Cirrhosis Management of people with cirrhosis primarily revolves around 2 main components- first managing the etiology causing it and other managing the complications arising due to cirrhosis. All the complications arising due to cirrhosis require specific management. In general, the main treatments include reducing salt from your diet and taking a type of medicine called a diuretic. For people developing liver cirrhosis due to excessive consumption of alcohol abstinence is the cornerstone of therapy. Patients who are unable to abstain from alcohol are shown to have significantly low 5 year survival. Occasionally patients with alcoholic cirrhosis have been shown to benefit from the use of glucocorticoids or oral pentoxifylline (drug causing decrease in pro inflammatory cytokines). For patients developing cirrhosis due to viral etiologies antiviral drugs have shown to benefit. For Hepatitis B virus Entecavir or tenofovir are useful, and for patients with cirrhosis due to Hepatitis C Virus direct antivirals have replaced the use of pegylated interferon and ribavirin. For patients developing cirrhosis due to autoimmune inflammation of the liver, immunosuppressive therapies are useful. UDCA is shown to help cirrhotic patients with etiology of biliary stasis. Managing complications arising due to cirrhosis revolves around managing complications of portal hypertension. The measures revolve around managing portal hypertension and ascites. In people with advanced cases of liver cirrhosis, a liver transplant may be the only treatment option as the liver may not be functional. Make sure to follow your doctor's advice and get all tests done as advised.














 WhatsApp
WhatsApp