Latest Blogs
Dehydration - Symptoms, Causes, Risk and Prevention
Body dehydration symptoms occur when you lose more fluid than you take in. In such cases, the body doesn't have enough water to carry out its functions normally. This necessitates that you replace the loss of fluids to control or prevent dehydration. And while any normal and healthy human being can become dehydrated, young children and older adults are at a higher risk. What are Dehydration Symptoms? Some may think that feeling excessively thirsty may be one of the first signs of dehydration. But it is not necessarily so. Many people don't even feel thirsty until after becoming dehydrated. This is why they say that you need to drink a lot of water to stay hydrated, especially during extremely hot weather. Dehydration Symptoms by Age Children experience more severe dehydration symptoms than adults. Some of the most common dehydration symptoms in children include: Mouth or tongue dryness Drying up of tears In infants, no wet diapers for as long as 3 hours Sunken cheeks Irritability Soft spot on top of the skull Sunken eyes In adults, the dehydration symptoms are as follows: Feeling extremely thirsty Seldom urination Dark urine Fatigue Feeling dizzy Disorientation It is advisable to see a doctor if you have been suffering from diarrhoea for more than 24 hours and are unable to retain fluids in your body. Causes of Dehydration Many a time, dehydration may occur for very simple reasons, like not drinking enough water. But there are other more serious causes that may result in dehydration symptoms. These are as follows: Diarrhoea: Sudden onset of severe and acute diarrhoea can result in severe fluid loss, including water and electrolytes, in a very short span of time. On top of this, if you are also vomiting, then it means more loss of fluids and minerals. This is bound to lead to dehydration. Fever: High fever is usually accompanied by dehydration. If you are also vomiting and suffering from diarrhoea along with the fever, then the problem of dehydration might worsen. Profuse sweating: Sweating is another way in which the body loses water along with ejecting toxins. If you are sweating too much and not drinking enough water to replace the lost fluid, then you might get dehydrated. This is hastened in very hot and humid weather. Excessive urination: Uncontrolled or undiagnosed diabetes may lead to an increase in the frequency of urination. This results in a loss of more fluids than the body should eject. Also, there are certain medications, like those used to control blood pressure, that also heighten the frequency of urination, resulting in dehydration. Risk Groups Anyone can start showing dehydration symptoms. But certain groups of people are at a higher risk. Children and Infants This is one category of people that experience severe dehydration symptoms. They are more prone to suffering from diarrhoea and vomiting, which is why the chances of getting dehydrated are higher. The fact that they have a higher surface-to-volume area also results in a higher loss of fluids from fever and burns. Because infants can't communicate clearly when they are thirsty, they spend long hours staying dehydrated. Older Adults With age, the body's fluid reserve shrinks. Your sense of thirst and ability to conserve water in your body also goes down. The problem heightens if you suffer from chronic illnesses like dementia or diabetes, or if you are on certain medications that cause body dehydration symptoms. In some elderly adults, mobility also becomes restricted, which means they can't get up and fetch water for themselves whenever they like. Chronically ill Adults People with undiagnosed or uncontrolled diabetes are at a very high risk of being dehydrated. Kidney diseases can also increase this risk. If your kidneys are affected, chances are that you will not have the urge to eat or drink, which has a direct impact on the fluid content in your body. People Exposed to Heat People who work outside in very hot and humid conditions can get severely sick and become dehydrated very quickly. The humidity in the air doesn't allow the sweat to evaporate and the body to cool down quickly. This results in an increased body temperature, which demands more fluids stored in the body. Prevention of Dehydration Dehydration symptoms are very much treatable and controllable. You can easily prevent becoming dehydrated by drinking plenty of water and fluids and consuming foods rich in water content. A few simple things you can do in addition to drinking water are as follows: Be aware of the symptoms of dehydration and pay attention to them. Drink water regularly, ideally before you start feeling thirsty. If you exert yourself too much physically, like during a workout, make sure to drink the right amount of fluids before, during, and after exercise. Keep checking the colour of your urine when you feel like you might be experiencing body dehydration symptoms. Don't limit your water intake during the day; the bodily fluid requirements vary from one person to another, and there is no one-size-fits-all solution. Increase your fluid intake during hot summers and humid weather. Get yourself checked to assess your risk for dehydration. Supplement your diet with water-rich foods such as fruits and vegetables. Add electrolyte supplements to your daily routine if you feel the need. If need be, set yourself fixed hours to drink water throughout the day. Remember that dehydration symptoms may come and go. But if they are not checked and treated, they may result in severe damage to your body.
Food Allergy Rashes: Causes, Treatments, and Natural Remedies
What are Food Allergy Rashes? Food allergy rashes are skin reactions that occur after eating certain foods. The rash may be itchy and red and can occur on any body part. Food allergies are caused by an immune system response to a food protein that the body perceives as harmful. In 2021, it was estimated that 32 million Americans would have food allergy rashes, including 5.6 million children. There are different types of food allergy rashes, each with its symptoms. The most common food allergy rash is atopic dermatitis, also known as eczema. Eczema is a chronic, inflammatory skin condition that causes dry, itchy skin. Food allergies can also cause hives, also known as urticaria. Hives are raised, and red welts on the skin can be itchy or painful. They are often caused by an allergic reaction to a food or medication. Other less common food allergy rashes include contact dermatitis and angioedema. Food allergies are common in children, and most go away independently. Although this is not always the case, food allergies generally outgrow in children. Food allergies can also happen later in life, but they are unusual. While you may feel symptoms of other diseases, your body's reaction to the poisoning will be unique. However, different types of food allergy rashes on the body are typical indicators, and their symptoms include: tingling in the mouth itching swelling of the lips, tongue, or throat wheezing or difficulty breathing nausea and vomiting abdominal pain or cramps Food Allergy Rashes Causes According to the American College of Allergy, Asthma and Immunology, children's most frequent food allergies are milk, eggs, and peanuts. According to experts, children outgrow milk, egg, soy, and wheat allergies at a rate of up to 25%. Peanut allergies, in particular, appear to be on the decline. In addition to wheat, numerous European countries have additional top allergens, including sesame, celery, lupin (a legume), and mustard. In the United States, sesame is becoming increasingly frequent. The body’s immune system mistakenly identifies a harmless food protein as a threat in people with food allergies. When the person eats the offending food, the immune system overreacts and releases chemicals that cause symptoms. The most common food allergens are proteins found in eggs, milk, peanuts, tree nuts, soy, wheat, fish, and shellfish. Food Allergy Rashes Treatments The best food allergy rashes treatment is to avoid the offending food. This can be difficult, especially if you’re allergic to everyday food items like milk or wheat, which are ubiquitous. If you have a severe allergy, you may need to carry an epinephrine auto-injector (such as an EpiPen) with you at all times in case of accidental exposure. For severe allergies, your doctor may prescribe a corticosteroid such as prednisone. Corticosteroids can be taken orally or injected. They are generally safe but can have side effects such as weight gain and mood swings. If you have a mild allergy, your doctor may recommend antihistamines to relieve symptoms. Antihistamines can be taken orally or applied topically (to the skin). However, they don’t work for everyone and may cause drowsiness. The following tests can help the doctor diagnose a food allergy: Blood test: This test looks for antibodies specific to certain food proteins, indicating an allergy. For instance, if you're allergic to peanuts, the test may reveal high levels of antibodies to a peanut protein called Ara h 2. Food diary: The individual records everything they eat and describes any emerging symptoms. For instance, if you think you're allergic to eggs but don't experience any symptoms after eating them, you're likely not allergic. Physician-supervised blinded oral food challenge: A food allergy can be very difficult to diagnose, especially in children. A physician administers a suspected food allergen in increasing doses to the individual over time, with close monitoring for symptoms. This method eliminates the risk of psychosomatic reactions. Food Allergy Rashes Natural Remedies Several natural remedies can help relieve symptoms of food allergy rashes. Some of them are: 1. Probiotics Probiotics can help reduce inflammation and improve gut health. They are available in supplements or fermented foods such as yoghurt and sauerkraut. Probiotics are live microorganisms similar to the beneficial bacteria found in the gut. 2. Vitamin C Vitamin C is a powerful antioxidant that can help reduce inflammation. Vitamin C supplements are widely available, or you can get your daily dose from foods such as oranges, strawberries, bell peppers, and broccoli. 3. Ginger Ginger is a well-known remedy for nausea and vomiting. It can also help relieve inflammation and pain. Ginger is available in supplement form or as a spice that you can add to your food. 4. Quercetin Quercetin is a plant compound that has anti-inflammatory and antioxidant properties. You can find quercetin in supplements and food items such as onions, apples, and green tea. 5. Butterbur Butterbur is a plant that has been used for centuries to treat various ailments, including allergies. Butterbur extract is available in supplement form and is effective in treating seasonal allergies. 6. Bromelain Bromelain is an enzyme found in pineapples that has anti-inflammatory properties. Bromelain supplements are often taken to reduce inflammation and swelling associated with injuries, surgery, and inflammatory conditions such as arthritis. Conclusion People often have allergic responses to specific allergens, such as pet dander and pollen, as well as compounds in foods, beverages, and personal hygiene products. The source determines the best way to treat an allergic reaction, although most minor instances may be treated with OTC antihistamine and anti-itch medicines. If you have been diagnosed with chronic or severe food allergy rashes symptoms, such as throat swelling or a change in heart rate, you should go to the hospital immediately. Anaphylaxis must always be treated as a medical emergency. Are you willing to know whether you're intolerant to any food? Take our Food Intolerance Test and find out for sure! Accurate and reliable, our test can detect up to 140 different food intolerances and is vegetarian-friendly. So why not give it a try today?
Iron Deficiency Anemia: Causes, Symptoms and Diagnosis
Iron is an essential nutrient for the body's general growth and development. In addition, it serves vital activities like oxygen transport, DNA synthesis, and muscle metabolism. Iron is essential when your body is growing, transforming, or changing. Lack of iron in the diet and increased demand in the body are common causes of iron deficiency in pregnancy and pediatrics. Iron deficiency can result in anemia, which lowers your hemoglobin levels. According to WHO figures, anemia affects 33% of non-pregnant women, 40% of pregnant women, and 42% of children globally. A lack of iron does not pose a threat to life. However, it might cause serious health issues. For instance, it results in dyspnea and exhaustion. The good news is that an iron-rich diet and supplementation can effectively prevent an iron deficiency. Causes of Iron Deficiency Anemia As its name suggests, iron deficiency anemia is caused by a lack of iron, blood flow, and a lack of iron-rich foods in the diet. Below are common causes of iron deficiency anemia. Increased Iron Demand The body's need for iron changes during the different phases of a person's life. For example, the years between childhood and adolescence are vital for growth. As a result, you must ensure you're getting enough iron-rich meals. Additionally, the need for iron rises during pregnancy; this is the prime cause of iron deficiency anemia in pregnancy. Low Absorption Of Iron Several conditions and surgical procedures may hinder iron absorption. For example, Crohn's disease and celiac disease are common causes of iron deficiency anemia. In addition, gastric bypass patients may not be able to absorb iron. These issues might prevent the gut from absorbing iron. Blood Loss Blood loss is among the common causes of iron deficiency anemia in adults. For instance, it could be brought on by blood loss from an injury, menstruation, etc. According to studies, conditions including gastric ulcer, hernia, and colorectal cancer can cause internal bleeding. In addition, heavy periods of women may be more likely to develop anemia. Diet The most common cause of iron deficiency anemia in children and adults is diet. A variety of nutritional factors affect how well iron is absorbed. Non-heme iron, which is of low quality, is present in vegetarian and vegan meals. Heme iron is present in non-vegetarian sources, in contrast. The rate of absorption is higher for heme iron. Vitamin C It is a necessary nutrient for the absorption of iron. Therefore, foods high in vitamin C may transform iron into a readily absorbable form. As a result, a deficiency in foods high in vitamin C is a common cause of iron deficiency anemia in adults. Phytates Some antinutrients interfere with non-heme iron absorption. For example, soybeans, black beans, lentils, split beans, mung beans, unrefined rice, cereals, and mung beans all contain phytates, which are antinutrients. When combined with iron-rich foods, they reduce your iron absorption. Calcium Although the exact mechanism is still unclear, experts think calcium prevents both heme and non-heme iron from being absorbed. Excess calcium causes iron deficiency anemia in pediatrics. Children who consume an excess of cow milk lack iron and have excess calcium, contributing to iron deficiency anemia. Symptoms of Iron Deficiency Anemia Depending on the severity, iron deficiency symptoms can vary. The list of iron deficiency symptoms is provided below. Fatigue Shortness of Breath Irregular Heartbeat/Palpitations Compromised Immune Health Pale Skin Hairfall Sore Mouth Headaches Spoon-Shaped Nails Diagnosis of Iron Deficiency Anemia Anemia can be easily detected through a complete blood count (CBC) with peripheral smear. Through this test it is possible to identify type of anemia and it may further give a clue to do further supplemental tests like i.e., serum iron studies, vitamin levels and identification of abnormal hemoglobinopathy for arriving at the correct diagnosis for the patient. Prevention of Iron Deficiency Anemia Good eating habits can help you avoid iron deficiency. Iron levels in the body may rise with the consumption of iron-rich meals. Here’s some simple dietary advice that can enable you to prevent iron deficiency anemia. Meat Iron content is exceptionally high in poultry and fish. Salmon and tuna are two more types of meat that are high in iron. To combat an iron shortage, incorporate one of these into your diet two or three times per week. Meat sources have a higher absorption rate of iron than plant sources. Eggs Iron, protein, and vitamins are all found in abundance in eggs. For example, about 9.7% of iron is present in every 100 grams of egg. Legumes Lentils are an excellent source of iron for vegetarians. Lentils provide abundant iron; eat it in salad or dal. Fruits and nuts Dry fruits like apricots are a rich source of iron. Iron can also be found in nuts, seeds, beans, tofu, and iron-fortified cereals. Vitamin C Iron absorption requires vitamin C. Vegetarian sources are rich in non-heme iron. They can eat it. Citrus fruits, bell peppers, and broccoli are food sources of vitamin C. Hydration Did you know drinking water is a reliable method of preventing human iron deficiency anemia? Researchers say drinking water locally enriched with iron compounds should be considered and used as a globally accessible means of controlling iron-deficiency anemia. Leafy Greens Leafy greens, such as spinach and kale, are a rich source of folate, which is necessary to avoid anemia. Additionally, leafy vegetables may further improve general wellness. Avoid Antinutrients Antinutrients can impede the absorption of iron. As a result, you should refrain from pairing meals high in iron with antinutrients like tea, coffee, and dairy products. These foods have antinutrients such as tannins, oxalic acids, and phytic acids that bind to iron and stop it from being absorbed. Don't combine calcium and iron-rich foods It is well known that calcium and iron vie for the same receptors. Therefore, according to experts, calcium and iron-rich diets prevent the body from absorbing iron. Conclusion Although iron deficiency is common among people due to poor eating habits, it can also be brought on by non-dietary practices. Iron deficiency is the main contributor to anemia. Healthy eating practices are crucial as a result. Follow the simple food recommendations detailed in the article to prevent iron deficiency and have an overall healthy life. But always remember to get advice from a professional before adding iron supplements. If you experience any symptoms, get the Anemia Profile-Maxi Test for accurate diagnosis.
The Science and Signs of Vitamin B6 Deficiency
A deficiency in vitamin B6 can have a range of health implications, leading to various symptoms and complications. However, there are also more specific symptoms for each type of vitamin B6 deficiency. This article delves into the causes, symptoms, diagnosis, and vitamin B6 deficiency treatment, providing a comprehensive understanding of this essential nutrient and its significance for overall health. What is Vitamin B6 Deficiency? Vitamin B6, also known as pyridoxine, is a vital water-soluble nutrient that plays a crucial role in various bodily functions. It is involved in the metabolism of amino acids, the synthesis of neurotransmitters, and the production of red blood cells. Vitamin B6 deficiency, also known as pyridoxine deficiency, is a condition that occurs when the body does not have enough vitamin B6. Vitamin B6 is a water-soluble vitamin, meaning it is not stored in the body and must be obtained from the diet. Signs & Symptoms of Vitamin B6 Deficiency Here are some standard and less common symptoms associated with vitamin B6 deficiency, including neurological, dermatological, and gastrointestinal symptoms. Common vitamin b6 deficiency symptoms include: Neurological Symptoms Vitamin B6 deficiency often first presents with neurological symptoms. Peripheral neuropathy is a common consequence, resulting in tingling or numbness in the extremities, particularly the hands and feet. Depression: A lack of vitamin B6 can affect neurotransmitter synthesis, potentially leading to symptoms of depression, mood swings, and irritability. Dermatological Symptoms Seborrheic Dermatitis: This skin condition can cause red, itchy, and scaly rashes on the face, ears, and other body areas. Cheilosis: Cracks and sores may develop at the corners of the mouth, a condition known as cheilosis. Gastrointestinal Symptoms Glossitis: Inflammation of the tongue, known as glossitis, can result from a deficiency in vitamin B6. This can lead to a sore, red, and swollen tongue. Stomatitis: Inflammation of the mouth and ulcers in the oral mucosa, referred to as stomatitis, can cause pain and discomfort when eating or speaking. Hematological Symptoms Anaemia: Vitamin B6 is necessary for producing haemoglobin, the protein that carries oxygen in red blood cells. A deficiency can lead to a type of anaemia known as sideroblastic anaemia, characterized by fatigue and weakness. Cognitive and Behavioral Symptoms Confusion and Cognitive Impairment: Vitamin B6 synthesizes neurotransmitters, which play a critical role in cognitive function. Deficiency can result in disorder and cognitive impairment. Irritability and Anxiety: Mood changes, irritability, and anxiety may be observed in individuals with a vitamin B6 deficiency. Weak Immune System: A lack of vitamin B6 can weaken the immune system, making individuals more susceptible to infections and illnesses. Cardiovascular Symptoms: Elevated levels of homocysteine in the blood may occur with a deficiency of vitamin B6. These elevated homocysteine levels are associated with an increased risk of cardiovascular disease. Seizures: In severe cases of deficiency, seizures may occur, particularly in infants with inborn errors of metabolism affecting vitamin B6 utilization. Signs of Vitamin B6 deficiency include Skin problems : A scaly rash around the mouth, nose, and eyes is a common sign of vitamin B6 deficiency. Other skin problems that may occur include cracks in the corners of the mouth (cheilosis), inflammation of the lips (cheilitis), and a red, greasy rash on the scalp, face, neck, and upper chest. Inflammation of the tongue : A swollen, sore, and red tongue, a condition called glossitis, is a common sign of vitamin B6 deficiency. Mouth Ulcers: Inflammation of the mouth and the development of ulcers in the oral mucosa, known as stomatitis, can cause discomfort and pain when eating or speaking. Causes of Vitamin B6 Deficiency Some of the most common Vitamin B6 deficiency causes include: People with a minimal diet or who avoid certain foods, such as meat, poultry, fish, and whole grains, may be at risk for vitamin B6 deficiency. Certain medical conditions, such as kidney disease, celiac disease, and inflammatory bowel disease, can interfere with the absorption of vitamin B6. Alcohol can interfere with the absorption of vitamin B6 and increase the body's need for vitamin B6. Pregnant and lactating women need more vitamin B6 than non-pregnant women. This is because vitamin B6 is essential for the development of the fetus and the production of breast milk. Other less common vitamin B6 deficiency causes include Genetic disorders: Some rare genetic diseases can affect how the body absorbs or uses vitamin B6. Tumours: Certain tumours can produce enzymes that break down vitamin B6. Hemodialysis: Hemodialysis is a medical procedure that removes waste products from the blood when the kidneys malfunction. Hemodialysis can also remove vitamin B6 from the blood. Effects of Long-term Vitamin B6 Deficiency Long-term vitamin B6 deficiency can have several serious health consequences. For instance: Long-term vitamin B6 deficiency can weaken the immune system and make people more susceptible to infection. Vitamin B6 is essential for brain health. This vitamin B6 deficiency can lead to cognitive impairment, such as problems with memory, attention, and learning. Increased risk of heart disease and stroke due to high levels of homocysteine in the blood, caused by vitamin B6 deficiency. This is because vitamin B6 is involved in the metabolism of homocysteine, an amino acid that can damage blood vessels. How is Pyridoxine Deficiency Diagnosed? Pyridoxine deficiency is diagnosed based on a person's medical history, physical examination, and blood tests. The doctor will ask about the person's diet, medications, and medical conditions. They can also perform a physical examination to look for signs of vitamin B6 deficiency, such as a scaly rash around the mouth, nose, and eyes, numbness and tingling in the hands and feet, and muscle weakness. Moreover, the doctor may order blood tests to measure vitamin B6 levels. If the blood tests show that the person has low levels of vitamin B6, the doctor will likely diagnose pyridoxine deficiency. Sometimes, the doctor may order other tests as well to determine the underlying pyridoxine deficiency causes. For example, the doctor may order tests to check for kidney disease, celiac disease, or inflammatory bowel disease. Here are some of the blood tests that may be ordered for pyridoxine deficiency diagnosis: Plasma pyridoxal 5'-phosphate (PLP) level: PLP is the active form of vitamin B6. A low PLP level is the most sensitive indicator of vitamin B6 deficiency. Erythrocyte pyridoxal 5'-phosphate (E-PLP) level: E-PLP measures vitamin B6 levels in red blood cells. A low E-PLP level is a good indicator of long-term vitamin B6 deficiency. Plasma Homocysteine Level: Homocysteine is an amino acid that can damage blood vessels. High levels of homocysteine are associated with vitamin B6 deficiency. What Should You Eat to Overcome Vitamin B6 Deficiency? To overcome vitamin B6 deficiency, you should eat a balanced diet that includes a variety of foods rich in vitamin B6. These include: Bananas, avocados, potatoes, leafy green vegetables, and citrus fruits Whole grains, such as brown rice, quinoa, and oats Lean protein sources, such as chicken, fish, beans, and lentils Almonds, walnuts, and sunflower seeds are all excellent sources of vitamin B6. Dairy products, such as milk, yoghurt, and cheese, are also good sources of vitamin B6. How Long Does It Take to Overcome Vitamin B6 Deficiency? It is important to note that overcoming vitamin B6 deficiency diseases can take time. Therefore, it is essential to be patient and consistent with your vitamin B6 deficiency treatment plan. In most cases, vitamin B6 deficiency can be overcome within a few weeks to a few months. However, people with severe vitamin B6 deficiency or an underlying medical condition may need to take a vitamin B6 supplement for a more extended period. Here are some ways to overcome vitamin B6 deficiency: Eat a balanced diet that includes a variety of vitamin b6 foods. Take a vitamin B6 supplement if recommended by your doctor. Avoid alcohol and tobacco. Get regular exercise. Manage any underlying medical conditions contributing to your vitamin B6 deficiency. Conclusion If you are experiencing any signs and symptoms of vitamin B6 deficiency, it is vital to see a doctor to get a diagnosis and treatment. Vitamin B6 deficiency treatment includes a dose of vitamin B6 supplement. However, in some cases, the underlying cause of the deficiency will also need to be treated. So, get yourself tested for deficiency with an at-home collection service by Metropolis and get an accurate health status today!
Cholesterol Levels - What You Need to Know
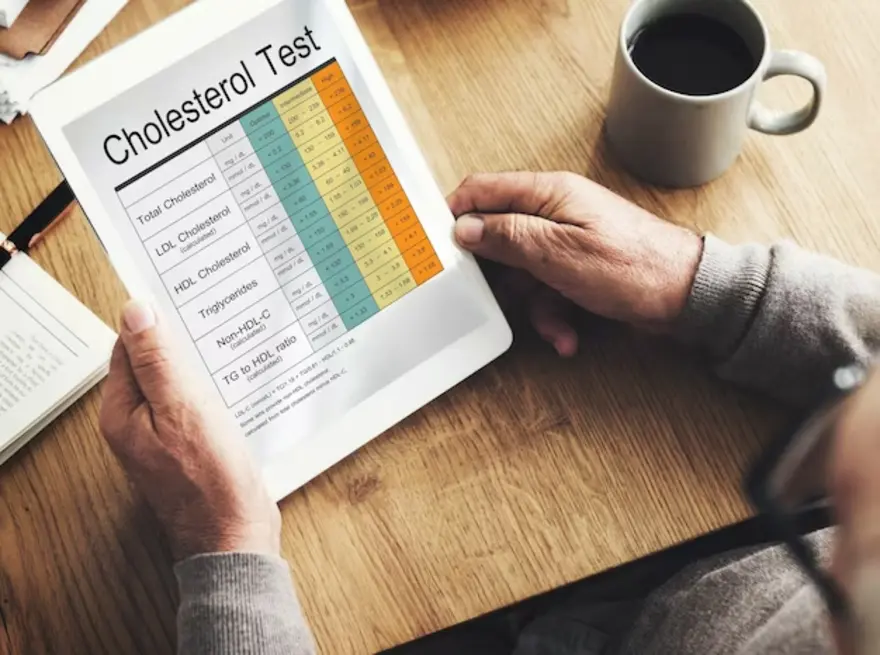
Cholesterol is a waxy substance found in your body and certain foods. It plays a crucial role in various bodily functions, but too much "bad" cholesterol (LDL) can increase the risk of heart disease. "Good" cholesterol (HDL) helps remove excess LDL. Managing cholesterol levels through a healthy lifestyle, diet, and, if necessary, medication is vital for heart health. Read more to know about other factors of Cholesterol and the required total cholesterol normal value. You will also learn about the other cholesterol values in the body. What is meant by Cholesterol? Cholesterol is a waxy, fat-like substance that's found in all the cells in your body. Your body needs cholesterol to make hormones, vitamin D, and substances that help you digest foods. Your body makes all the cholesterol it needs but you also get extra cholesterol from the foods you eat. Your body has a system for getting rid of excess cholesterol but too much cholesterol in your blood can raise the risk of heart disease and stroke. This is because cholesterol can build up in the walls of your arteries, forming plaques. These plaques can narrow or block your arteries, making it difficult for blood to flow to your heart and brain. How do you measure cholesterol levels? Cholesterol levels are measured with a blood test called a Lipid Panel. This test measures LDL cholesterol, HDL cholesterol, triglycerides, and total cholesterol range in your blood. To prepare for a lipid panel, you must fast for 9-12 hours before the test. This means not eating or drinking anything but water during that time. During the test, a healthcare professional will draw blood from a vein in your arm. The blood will be sent to a laboratory for analysis. Your lipid panel results will be available within a few days. Your doctor will review your results and discuss any necessary lifestyle changes or medications. Here are the steps involved in measuring cholesterol levels: Fast for 9-12 hours before the test. Have a blood sample drawn from a vein in your arm. Send the blood sample to a laboratory for analysis. Review the results with your doctor. What are the types of cholesterol? There are two main types of cholesterol: Low-density lipoprotein (LDL) cholesterol: LDL cholesterol is known as "bad" cholesterol because it can build up in the walls of your arteries. It can lead to hardening of the arteries (atherosclerosis), which can increase the risk of heart disease and stroke. The LDL normal value is less than 100 mg/dL (3.4mmol/L). High-density lipoprotein (HDL) cholesterol: HDL cholesterol is known as "good" cholesterol because it helps to remove LDL cholesterol from the arteries. This helps to keep the arteries clear and reduces the risk of heart disease and stroke. The HDL normal value is 40 mg/dL (1mmol/L) or more. There are other types of cholesterol listed below- Very low-density lipoprotein (VLDL) cholesterol: VLDL cholesterol is a type of fat made in the liver and released into the bloodstream. VLDL cholesterol is converted to LDL cholesterol in the bloodstream. Intermediate-density lipoprotein (IDL) cholesterol: IDL cholesterol is formed when VLDL cholesterol loses some of its triglycerides. IDL cholesterol can be converted to LDL cholesterol or HDL cholesterol. Lp(a) cholesterol: Lp(a) cholesterol is a type of cholesterol that is similar to LDL cholesterol, but it has an additional protein attached to it. Lp(a) cholesterol can build up in the walls of the arteries and increase the risk of heart disease and stroke. What do your cholesterol numbers mean? Your cholesterol numbers can help you understand your risk of heart disease and stroke. The four main cholesterol numbers are: Total cholesterol: This is the total amount of cholesterol in your blood. LDL cholesterol: This is the "bad" cholesterol that can build up in your arteries and form plaques. HDL cholesterol: This is the "good" cholesterol that helps remove LDL cholesterol from your arteries. Triglycerides: This is another type of fat in your blood that can raise your risk of heart disease and stroke. Here is a breakdown of what your cholesterol numbers mean: Total cholesterol range- Average: Less than 200 milligrams per deciliter (mg/dL) Borderline high: 200-239 mg/dL High: 240 mg/dL and higher LDL cholesterol range- Optimal: Less than 100 mg/dL Near-optimal: 100-129 mg/dL Borderline high: 130-159 mg/dL High: 160-189 mg/dL Very high: 190 mg/dL and higher HDL cholesterol range- Low: Less than 40 mg/dL in men and less than 50 mg/dL in women Ideal: 60 mg/dL or higher in men and 55 mg/dL or higher in women Triglycerides range- Normal: Less than 150 mg/dL Borderline high: 150-199 mg/dL High: 200-499 mg/dL Very high: 500 mg/dL and higher What is the normal serum cholesterol level? Total cholesterol normal value for adults: Less than 200 mg/dL LDL cholesterol normal range value: Less than 100 mg/dL HDL cholesterol normal range value: 40 mg/dL or higher Triglycerides: Less than 150 mg/dL How often should you get your cholesterol checked? The frequency with which you should get your cholesterol checked depends on your age and risk factors for heart disease and stroke. The American Heart Association recommends that adults aged 20 or older have their cholesterol checked every four to six years. However, if you have any of the following risk factors, you may need to get your cholesterol checked more often: Age 45 or older (men) or 55 or older (women) Family history of heart disease or stroke High blood pressure Diabetes Smoking Obesity High triglycerides Low HDL cholesterol Suppose you have other risk factors for heart disease, such as high cholesterol, low HDL cholesterol, or high triglycerides. In that case, your doctor may recommend checking your cholesterol even more often. It is also essential to talk to your doctor about how often you should check your cholesterol if you take any medications affecting cholesterol levels, such as statins or niacin. What affects your cholesterol levels? Your cholesterol levels are affected by several factors, including: Unhealthy Diet: Eating high in saturated and trans fats can raise cholesterol levels. Saturated fats are found in animal products, such as red meat, butter, and full-fat dairy products. Trans fats are found in processed foods, such as fried foods and baked goods. It is essential to eat a diet that is low in saturated and trans fats and high in fruits, vegetables, and whole grains. Lack Of Exercise: Exercise can help lower your cholesterol levels. Aim for at least 30 minutes of moderate-intensity exercise most days of the week. Weight: Being overweight or obese can raise your cholesterol levels. Losing weight can help lower your cholesterol levels. Smoking: Smoking can raise your LDL cholesterol value levels and lower your HDL cholesterol value levels. Quitting smoking can help improve your cholesterol levels. Medical conditions: Certain medical conditions, such as diabetes, high blood pressure, and kidney disease, can raise cholesterol levels. Medications Consumed: Certain medications, such as statins and niacin, can raise cholesterol levels. Age: As you get older, the LDL cholesterol range by age changes and levels tend to rise. Gender: Men people tend to have higher LDL and lower HDL cholesterol levels than women. Normal cholesterol levels for women may be different. Genetics: Your cholesterol levels can also be affected by your genes. How can you lower your cholesterol? Eat a healthy diet: This means eating a diet low in saturated and trans fats and high in fruits, vegetables, and whole grains. Saturated fats are found in animal products, such as red meat, butter, and full-fat dairy products. Eat fruits, vegetables, whole grains, beans, lentils, nuts, seeds, fish, olive oil, and avocados. Exercise regularly: Aim for at least 30 minutes of moderate-intensity exercise most days. Exercise can help raise your HDL cholesterol levels and lower your LDL cholesterol levels. It can also help you maintain a healthy weight. Perform walking, running, biking, swimming, dancing, and gardening. Maintain a healthy weight: Being overweight or obese can raise your cholesterol levels. Losing weight can help lower your cholesterol levels. Even a tiny amount of weight loss can make a difference. Quit smoking: Smoking can raise your LDL cholesterol levels and lower your HDL cholesterol levels. Quitting smoking can help improve your cholesterol levels and reduce your risk of heart disease and stroke. Manage other medical conditions: If you have other medical conditions, such as diabetes, high blood pressure, or kidney disease, it is vital to manage them carefully. These conditions can raise your cholesterol levels, so managing them can help lower your cholesterol levels and reduce your risk of heart disease and stroke. Conclusion It is important to have your cholesterol levels checked regularly, especially if you have any risk factors for heart disease and stroke. If your cholesterol levels are high, talk to your doctor about how to lower them. With lifestyle changes and medication, you can lower your cholesterol levels and reduce your risk of heart disease and stroke. To learn more about how you check your cholesterol level, you can contact Metropolisindia’s professionals. They will provide you with the convenience of testing at home and the benefit of accurate test results
Difference Between Food Allergy and Food Intolerance
A food allergy is usually any unwanted symptomatic reaction to the food you consume. The reactions are usually immediate after the consumption of the allergen. However, all reactions cannot be termed as allergies, as such reactions and their symptoms can also be due to the intolerance of those foods to your physiology. Every individual’s physiology differs remarkably from one another, and the allergies or intolerances vary accordingly. Not to say that all individuals do show such symptoms. If your body suffers from signs and symptoms after having a food item, it is best to find out if it is a food allergy or food intolerance. It helps with a better understanding of how and what quantity of certain foods may be unhealthy for your physiology. Additionally, it also clears the path to choosing to treat the same. Food intolerance is usually a delayed systemic response of the body’s systems, which may even occur a few days or weeks after the consumption of a particular food item. To give you an idea and to start with understanding the differences between the two, you must observe the cause of such symptoms—if it is the repeated consumption of certain food items or your everyday food intake. Let’s get further into the meanings and differences between food allergy and intolerance for a detailed understanding of the two physiological aspects. The Causes and Symptoms of Food Allergies Food allergy is a condition that often surfaces due to the body’s immune system not working optimally. If your body suffers from a food allergy, it is likely because your immune system identifies the particular food item as a harmful, invading, foreign object, thus leading to a fight response. A hyperactive immune system thus results in several observable symptoms that you may find surfacing in and on the body. Often, an allergic reaction is due to the high release of histamines in the body, a chemical addressing a local immune response in the body. It is ideally a useful chemical enabling blood thinning for the WBCs to pass easily and reach the affected location, among other purposes. However, in the case of food allergies, the immune system’s overactive state leads to a release of histamine and other responsive chemicals in high quantities to counter such food’s impact. Such a sudden release of these chemicals leads to severe responses, which are allergic symptoms. A food causing allergy in one’s body is identified as an allergen. Common food products that turn out to be allergens for a remarkable number of people include peanuts, animal dander, pollen, seafood, among others. Common symptoms related to a food allergy that one might come across include the likes of - Itching in the body Breathing trouble due to constricted/inflamed lungs Excessive watery discharge from the eyes Swelling and congestion in the nose Diarrhoea and vomiting in severe cases Red rashes on the skin Pressure in the chest or pain Anaphylaxis in fatal conditions The Causes and Symptoms of Food Intolerance Unlike a food allergy, food intolerance is the body’s response to any uneasy or incompatible food, leading to indigestion or irritation of the digestive system. As a result, the body’s capacity to digest the food reduces, leading to signs and symptoms. To understand food intolerance, you must know that it is not as sudden as an allergy and takes time to surface. Managing food intolerance is a slow process, too, needing you to eliminate certain food items from the diet. The doctor may also administer some light medications for any potentially harmful intolerance symptoms to subside. Long-term plans for food exclusion are among the best ways to counter intolerance to certain food items in your day-to-day life. Common food items causing intolerance in the body include wheat, gluten, and milk, along with certain vegetables and fruits. You must have commonly heard of the term ‘lactose intolerance,’ which is the body’s intolerance to lactose present in milk and milk products, leading to gastrointestinal discomfort. Some common symptoms of food intolerance in your body include the following. Constipation, cramps, bloating, and similar symptoms in the stomach Redness or inflammation of the skin Acidity and heartburn Excessive dryness of the skin Acne and pimples Headaches Mood swings and irritability Primary Points of Difference Between Food Allergy and Food Intolerance Some common points of difference between a food allergy and food intolerance are listed below for a better understanding of the two conditions. 1. Biological systems impacted The body’s immunity is the biological system that impacts/leads to allergic reactions to a certain food when in close contact. In the case of intolerance to food, chemicals produced in the digestive system are primarily responsible for the symptomatic reactions. Depending on the chemical composition of the body’s physiology, any healthy food consumed can cause intolerance symptoms. 2 .Causes In the case of a food allergy, your body’s immune system tries to protect it from certain food items that it considers a threat to the overall health. An allergy can be very specific to individuals based on the allergenic behaviour of such food. Apart from food consumption, even the smell or touch of certain food can cause allergic reactions in the body. Some other causes of food allergy include family history, age, maturity of the digestive system, and asthma. The body’s Intolerance to food is, however, typically caused due to the body’s inability to process or digest certain food due to the lack of necessary chemicals or enzymes. The presence of specific chemicals in such food or the presence of food additives can also be intolerance triggers. Irritable bowel syndrome, celiac disease, and sensitivity to dried fruits are identified as other reasons for intolerance to food. 3. Diagnosis Food allergies are best diagnosed through dedicated blood tests, oral food tests, physical examinations of the skin, and tests based on food elimination. Additionally, the healthcare professional may inquire regarding your history of allergies, any family history of such conditions, etc. The first and basic test is usually a blood test to detect the Immunoglobulin E levels. If the levels are abnormal, further allergy testing like Allergy panels may be needed. There are now various tests available to detect food allergies like Allergy panel- Milk and milk products , Allergy panel- Fruits and other such tests. Apart from these basic blood tests like CBC, ESR may also be done to check certain abnormal parameters. Food intolerance is difficult to diagnose and most laboratories do not offer any test for it. Metropolis Healthcare Ltd. offers testing for food intolerance using protein array technology. Test has a comprehensive range and can detect IgG antibodies against 150 + foods. 4. Severity A food allergy may or may not be severe depending on your body’s reaction to the allergen identified. However, in some cases, an allergen may lead to severe symptoms, such as diarrhoea, vomiting, asphyxiation, etc. Most of these symptoms appear shortly after coming in contact with such food, like in the following 2 hours. Comparatively, food intolerance leads to low severity symptoms, which often appear over 4-5 hours after food consumption. 5. Time taken for recovery The recovery time from a food allergy often depends on the extent of exposure to such allergens and the severity of the symptoms observed. The higher the exposure and/or symptoms, the longer it takes to recover. Under food intolerance, however, eliminating the identified food from your diet can lead to a muted response of the body to such intolerance, resulting in long-term recovery. 6. Treatment Cases with mild symptoms of food allergy can be easily treated through antihistamine administration. Severe cases of allergy may need a more immediate, assertive, and aggressive response, such as hospitalisation or epinephrine injections. All these treatments must be done under the guidance of your doctor, though. As per research reports, there does not exist any definitive cure for the treatment of intolerance to various food items. The best bet has been to eliminate intolerant food items from one’s diet. Parting Thoughts With this detailed insight regarding the differences between food allergy and food intolerance, you should be better able to distinguish between the two as per the symptoms, severity, food consumption, and such factors. You may watch out for either of them if you feel itchy, discomfort, rashes, or any such symptoms after consuming a specific food.
Understanding Electrolyte Tests: Normal Range & Levels
Electrolytes are minerals like sodium, potassium, and chloride,, with electric charges controlling several vital functions. They enable the transport of nutrients into the cells and help remove the waste matter. An electrolytes panel or electrolyte test determines abnormal levels of electrolytes in the blood to diagnose multiple diseases and health conditions. What is an Electrolytes Test? We know that the total water content in a healthy adult human body is about sixty per cent. Fluids in our body comprise electrolytes. These are vital for regulating the body's fluid balance and stabilising the pH level. In fact, electrolytes are helpful in maintaining heart rhythm, muscle movements, and nerve activities. Electrolytes are present in various body fluids like blood, sweat, and urine. These comprise: Sodium- Facilitates the body's fluid control and enables proper activities of muscles and nerves. Calcium- Besides building bones, calcium regulates heart rhythm, transmits nerve signals, and ensures muscle control. Phosphate- It plays a crucial role in moving compounds and molecules from cells. Magnesium- It boosts functions of the brain and muscles while helping cells to produce energy from nutrients. Chloride- It plays a vital role in the maintenance of a fluid balance between inside and outside the cell structure. Bicarbonate- It helps maintain the pH balance to prevent alkalosis and acidosis The term electrolyte has a close association with an electrical charge. An imbalance of electrolytes means your body cannot maintain balance at the basic chemical level. Electrolytes help cells conduct electricity, induce chemical reactions, and preserve the fluid balance between the inner and outer environment of cells. Electrolyte imbalance and related medical conditions Maintenance of the electrolyte balance is vital for the functioning of the body. Each electrolyte element has a specific role, and an imbalance can lead to different medical conditions requiring restoration of the electrolyte balance. Following are some conditions because of higher or lower electrolyte levels. Hyperkalemia- Excess potassium in the blood leads to arrhythmia, muscle weakness, and confusion. Hypokalemia- Low potassium levels can cause severe issues, including kidney damage. Hypercalcemia- The presence of higher levels of calcium in the blood can affect the heart, brain, and kidneys. It also causes digestive disorders and joint pain. Hypocalcemia- Low sodium levels in the blood may cause behaviour changes, confusion, muscle spasm, and loss of muscle control. Hypernatremia- Excess sodium in the blood causes behaviour issues, coma, or seizures. Hyponatremia- Insufficient sodium levels in the blood cause seizures, coma, confusion, and weak reflexes. Acidosis- Deficiency of bi-carbonate increases the acidity of the blood. This condition is known as acidosis. It may cause shortness of breath and confusion. Alkalosis- It is the opposite of acidosis. The blood becomes alkaline in alkalosis, with higher bicarbonate levels. It can cause muscle twitching and irregular heartbeats. Considering an Electrolytes Test There are conditions with vague symptoms like severe diarrhoea, vomiting, confusion, weakness, and irregular heartbeats. Physicians may order a serum electrolytes test if they suspect an electrolyte imbalance as the root cause. The electrolytes test involves taking out a blood sample from the individual's vein with a small needle. The test is not very painful as one may experience a minor sting-like sensation as the technician inserts the needle. No fasting is necessary before the electrolyte test unless your physician recommends additional tests like a fasting glucose test. Drink plenty of water to facilitate easy blood withdrawal. The test results will show the levels of electrolytes in mmol/L. The following are normal ranges of electrolytes: Potassium- 3.5 to 5.2 Sodium- 134 to 144 Chloride- 96 to 106 Bi-carbonate- 20 to 29 You need not panic if the results are not within the normal ranges, as several factors like medicines and dehydration can affect these values. Your physician will study the results of the electrolyte test. The main difference between positively charged and negatively charged electrolytes may suggest disorders of the kidneys or lungs. Depending on your medical history and clinical assessment, they may order additional tests if there is an electrolyte imbalance. Visit us for the electrolyte panel test! Highlights of Electrolyte Test The electrolyte panel test is another term for the Serum Electrolytes Test, which measures the body's electrolyte levels. A physician may order the test as part of a routine health check or to study the abnormal electrolyte levels to understand the underlying causes of irregular heart rhythm, hypertension, and kidney disorders. Measurement of Serum electrolytes may involve testing a particular electrolyte if the physician wants to check the level of a single electrolyte. Usually, the testing of common electrolytes is a routine procedure. Your physician will study the results to know the variance between normal and actual levels of different electrolytes. These levels may be normal, higher, or lower. The physician will correlate the results with other factors before reaching any conclusion. There are multiple reasons for abnormal electrolyte levels. These may not always be serious. Fluid loss because of diarrhoea or excessive sweating may cause an imbalance of electrolytes. Abnormal Serum electrolytes levels can be because of blood pressure medicines or antacids. Why does an individual need an Electrolyte Test? An electrolytes blood test is helpful in many situations since electrolytes play diverse roles in supporting and maintaining multiple functions. Besides ordering an electrolytes test as a routine screening test, a physician may suggest an electronic panel because: An electrolyte imbalance may involve problems in the liver and kidneys. The electrolyte panel helps monitor kidney and liver functions. It is also helpful to check the nutritional status and hydration if a physician suspects malnutrition or dehydration in a patient. An electrolyte test is helpful for checking brain health, as sodium is a significant electrolyte for a healthy brain. Calcium, potassium, and magnesium are vital electrolytes for proper heart functioning. The test is suitable for monitoring electrolyte levels in diabetes. An electrolyte blood test is suitable to assess nonspecific symptoms, such as appetite loss, dizziness, or fatigue. Physicians use the test to rule out specific endocrine, liver, and kidney conditions. The takeaway The electrolyte test helps assess body fluids. It provides a clear picture of different electrolyte levels in the blood along with the acid-base balance. A physician may order a serum electrolyte test to monitor the effectiveness of various treatments. The test helps understand the course of a specific medical condition. There are multiple causes of an electrolyte imbalance, including dehydration. An electrolyte test helps physicians arrive at a specific diagnosis or rule out a suspected disease. Electrolyte panel may also be a part of testing for other systems like Renal function tests and Comprehensive metabolic panel. Get in touch for a reliable electrolyte panel test!

















 WhatsApp
WhatsApp