Latest Blogs
Edema: Causes, Symptoms, and Effective Treatment
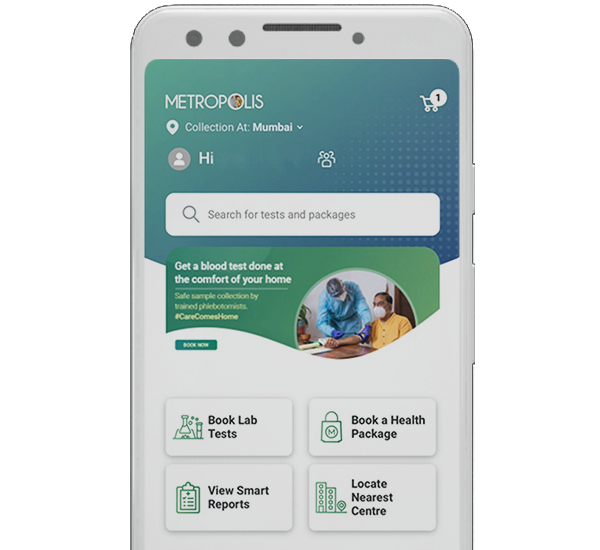
What is edema? Edema is known as a health condition where the body fluid is trapped in the body tissue, causing swelling. This condition is the most common in legs, ankles, and legs, but may occur in other parts of the body, such as the face, hands, and abdomen. Who does Edema affect? Edema can affect anyone, but it is more common in adults over 65 and pregnant women. Although common, the exact frequency is unknown because mild cases usually resolve on their own. Edema can interfere with daily activities due to increase in size or swelling in certain parts of the body. However, simple lifestyle changes, such as elevating the swollen area or moving around after sitting or standing for long periods of time, can reduce the edema symptoms. How common is Edema? Edema is a common condition that many people experience at some point in their lives. Mild, temporary edema is often harmless and goes away on its own. However, chronic or severe edema may indicate a more serious underlying condition that requires medical evaluation and treatment. How does Edema affect my body? Edema affects the body by causing swelling in the tissues due to excessive fluid retention. This swelling can lead to discomfort, decreased mobility, and changes in the appearance of the affected area. In severe cases, edema can affect organ function and circulation, possibly leading to complications such as skin ulcers or difficulty breathing. Treating the underlying cause of edema is essential to effectively manage symptoms and prevent further health problems associated with edema. What are the symptoms of Edema? Edema symptoms usually include swelling of the hands, arms, feet, ankles, and legs, often accompanied by a feeling of heaviness or tightness in the affected area. If pressure is applied, the skin may retain a dimple or pit (pitting edema). Other common edema symptoms include noticeable swelling of the skin, increased abdominal size or bloating, and difficulty putting on shoes or clothing due to swelling. In severe cases, edema symptoms may include stiff joints, stretched or shiny skin, and limited mobility. It is important to recognize these symptoms because they may indicate an underlying condition such as heart, kidney, or liver disease that requires medical examination and appropriate treatment to reduce discomfort and prevent complications. In severe cases, edema symptoms may include joint stiffness, stretched or shiny skin, and limited mobility. It is important to identify these symptoms as they may indicate the need for medical examination and treatment for underlying conditions like heart, kidney or liver as well as other possible diseases to reduce discomfort and prevent complications. What causes Edema? After diagnosing edema, your healthcare provider will try to identify the underlying cause of fluid buildup. The following are common edema causes: Gravity: Long periods of sitting or standing in one place can lead fluid to pull down into your arms, legs and feet (dependent edema). Weakened Valves: If the valves in your veins are weak, it becomes challenging for your veins to push the blood back up to your heart, which causes varicose veins and fluid buildup in the legs. Underlying Medical Conditions: Conditions such as heart failure, lung, liver, kidney and thyroid diseases often cause edema as a symptom. Medication Side Effects: Some medications used to treat blood pressure or pain may cause edema as a side effect. Poor Nutrition: Excessive salt consumption and an unbalanced diet can lead to water retention. Pregnancy: Pressure on blood vessels due to growing uterus can cause leg swelling during pregnancy. Compromised Immune System: An allergic reactions, infections, burns, traumas or clots can lead to edema. How is Edema diagnosed? A physical examination by a healthcare provider is essential to diagnose edema. They will check for swelling, especially where the skin looks shiny or stretched. Edema grading can be used for further evaluation. Here, the provider will press an area of raised skin for 5 to 15 seconds (pitting test). A dimple (pit) that appear indicates fluid accumulation. What is Edema grading? Edema grading is a way to classify the severity of swelling based on its depth, duration, and the effect it has on the surrounding tissues. It helps healthcare providers assess the extent of fluid accumulation and guide treatment decisions. Typically, edema grading involves several levels: Grade 1 (Mild): Barely perceptible swelling, usually identified by slight pitting when pressure is applied Grade 2 (Moderate): Noticeable swelling that persists longer, with deeper pitting that may last longer after pressure is removed Grade 3 (Severe): Significant swelling that causes pronounced pitting, often lasting for a prolonged period after pressure is released. This level may also include skin changes like a shiny appearance and difficulty with mobility. Grade 4 (Very Severe): Extreme swelling where pitting is profound and lasts for an extended time, potentially leading to skin ulceration and severe mobility issues. Healthcare professionals use these grades to monitor changes in edema over time and adjust edema treatment strategies accordingly, with the goal of reducing fluid buildup and alleviating edema symptoms effectively. How is Edema treated? Edema treatment is designed based on the root cause of the condition. For instance: In case of edema caused by lung disease, quitting smoking is advised. If chronic heart failure leads to edema, it is advised to change the lifestyle of weight, fluid and salt intake When medication side effects result in edema, adjustments may be made to drug dosages. To reduce edema swelling further, these steps can help: Elevate your legs above heart level when sitting or lying down. Avoid stationary standing or sitting for long periods and go on short walks. Wear support socks or stockings that exert pressure on body parts to prevent fluid collection. Reduce the amount of salt in your diet. Follow doctor’s advice for taking medications, such as diuretics which help rid your body of excess fluid. What can’t I eat with Edema? In some cases, edema can be the result of a high-salt diet. Since salt causes your body to retain water, which can leak into the tissues and cause swelling, reducing salt intake can help to relieve edema symptoms. How soon after treatment will I feel better? Depending on the causes of edema temporary or permanent. Swelling usually lasts a few days, with the worst swelling occurring in the first two days and decreasing by the third day. Timely edema treatment can help in effective management of the swelling. How can I prevent Edema? Edema can be prevented with regular exercise as it helps in preventing fluid buildup, and dietary adjustments to reduce salt intake. However, if the edema is caused by any of these underlying health conditions, such as heart failure, liver or kidney disease, management of symptoms is essential. What can I expect if I have Edema? If you experience edema or swelling in your body, be sure to consult your healthcare provider immediately. If this condition is not treated, the swelling will increase and can lead to serious health problems. The underlying condition causing the edema can be controlled with treatment, and lifestyle modifications can also help in reducing swelling and fluid buildup. Conclusion Understanding and managing edema is essential to maintain a healthy lifestyle. Although it may seem intimidating, it is completely manageable with right knowledge and medical care. Metropolis Healthcare offers comprehensive diagnostic services to help patients understand health problems such as edema through specific tests. The convenience of at-home sample collection by qualified technicians ensures stress-free experience while prioritizing your health.
Blood Cancer Symptoms Unveiled: Insights into Detection and Treatment
What is blood cancer? Blood cancer refers to cancers that affect the blood, bone marrow, or lymphatic system. These cancers disrupt the production and function of blood cells, which include red blood cells (carry oxygen), white blood cells (fight infections), and platelets (help blood clot). Types of blood cancer include leukemia (affects white blood cells), lymphoma (affects the lymphatic system), and myeloma (affects plasma cells). Blood cancer symptoms may include fatigue, unexplained weight loss, frequent infections, easy bruising or bleeding, and swollen lymph nodes. Blood cancer treatment options vary based on the type and stage of the cancer and may include chemotherapy, radiation therapy, targeted therapy, or stem cell transplantation. Are blood cancers serious? Blood cancer is a serious condition that can be life-threatening if not treated promptly. It disrupts the body's ability to produce healthy blood cells, leading to severe blood cancer complications such as infections, bleeding problems, and organ failure. What are the survival rates for blood cancer? Survival rates for blood cancer are based on averages. These vary depending on the type of blood cancer, but many people with blood cancer have the same life expectancy as most other people. It is important to note that blood cancer represents about 10% of all cancers diagnosed each year. The survival rates for these cancers have been steadily improving thanks to advances in medical science. What are the three types of blood cancer? The three main types of blood cancer are leukemia, lymphoma, and myeloma. Leukemia: Affects the blood and bone marrow, causing abnormal growth of immature white blood cells. These cells displace healthy blood cells, impair their function, and weaken the immune system. Lymphoma: Targets the lymphatic system, including the lymph nodes, spleen, and other organs that produce and store immune cells. It appears as tumors in the lymph nodes and can spread to other organs, affecting the body's ability to fight infections. Myeloma: Originates in plasma cells, it is a type of white blood cell that produces antibodies. Myeloma cells accumulates in the bone marrow, while disrupting the production of normal blood cells and weakening bones, leading to bone pain and fractures. Each type of blood cancer has distinct characteristics and requires tailored blood cancer treatment approaches, including chemotherapy, radiation therapy, targeted therapy, and stem cell transplantation, depending on the specific diagnosis and stage of the disease. What causes blood cancer? Blood cancer causes can be linked to mutations in the DNA of blood cells, but it is not known exactly why this happens. Environmental and genetic factors are believed to trigger DNA changes in leukemia. In lymphoma, changes in the genes of white blood cells cause them to multiply out of control. In myeloma, new genetic instructions cause plasma cells to proliferate in the bone marrow. What are blood cancer symptoms? Blood cancer symptoms can vary depending on the type and stage of the disease. The most common blood cancer symptoms include persistent fatigue, unexplained weight loss, frequent infections, easy bruising or bleeding, swollen lymph nodes, and night sweats. Other blood cancer symptoms of blood cancer includes bone pain or tenderness, stomach discomfort or feeling full, and general weakness or malaise. These blood cancer symptoms may results from disruption of normal blood cell production and function, as well as the impact of cancer cells on the body's immune system and organs. Early detection and diagnosis are crucial for initiating a timely treatment and improving the outcomes for individuals with blood cancer. How is blood cancer diagnosed? Blood cancer diagnosis usually involves several steps. Initially, a thorough medical history and physical examination are conducted to assess symptoms and signs suggestive of the disease. Blood tests, such as a complete blood count (CBC) and blood chemistry tests, help evaluate the levels of various blood cells and detect abnormalities. Further blood cancer diagnostic procedures may include: Bone Marrow Aspiration and Biopsy: A sample of bone marrow is taken from the hip bone using a needle to examine the presence of cancerous cells and assess the bone marrow's ability to produce normal blood cells. Imaging Tests: A CT scan, MRI scan, or PET scan may be used to assess how far the cancer has spread to the lymph nodes, organs, and bones. Lymph Node Biopsy: If lymph nodes are enlarged, a biopsy may be performed to examine lymphatic tissue for cancerous cells. Genetic Tests: Molecular testing can be done to detect specific genetic mutations or abnormalities to help guide treatment decisions. When a blood cancer is diagnosed, additional tests may be done to determine the type and stage of the blood cancer. This comprehensive approach allows healthcare providers to develop appropriate blood cancer treatment plans tailored to the individual's condition. How do healthcare providers treat blood cancers? Blood cancer treatment depends on the type, stage of the disease, and the patient's overall health. Common blood cancer treatments include chemotherapy to kill cancer cells, radiation therapy to target and shrink tumors, and stem cell transplants to replace diseased bone marrow with healthy stem cells. Targeted therapy drugs attack specific cancer cells without harming normal cells. Immunotherapy enhances the body's immune system to fight cancer. Supportive care such as blood transfusions, antibiotics, and medications to manage side effects like pain and nausea are essential. Blood cancer treatment plans are tailored to each patient to achieve the best possible outcome. What are the common side effects of blood cancer treatment? Different blood cancer treatments can have different side effects. Chemotherapy and radiation therapy might result in fatigue, hair loss and nausea among others. CAR T-cell therapy could cause cytokine release syndrome (CRS) and neurological issues while immunotherapy might lead to skin rashes and fatigue. How can I reduce my risk for developing blood cancer? While blood cancer prevention is difficult as the exact causes are unknown, researchers suggest avoiding radiation exposure and certain chemicals which might trigger genetic changes leading to blood cancer. Can blood cancer be cured? Curing blood cancer depends on numerous factors like the type of blood cancer, stage, patient’s health and more, advancements in medical science have significantly improved survival rates. However, the blood cancer complications can also impact the treatment outcomes and a long-term prognosis. Conclusion Understanding blood cancer is the first step towards managing it effectively. Awareness about its symptoms, causes, and treatment options can empower you for a proactive approach towards your health. If you suspect any blood cancer symptoms, consult with healthcare providers immediately for timely diagnosis and treatment. When you need expert diagnostic services, consider Metropolis Healthcare – a leading pathology lab known for their accurate testing and compassionate care. With their at-home blood sample collection service and advanced diagnostic labs, managing your health becomes more convenient than ever. Prioritise your health with the help of Metropolis Healthcare!
Albinism: Symptoms, Causes, Types, and Treatment Strategies
What is Albinism? Albinism is a group of genetic disorders characterized by little or no melanin production. People with albinism often have pale skin, hair and eyes. In addition to affecting physical appearance, albinism can also cause vision problems. What Does Albino Mean? The word Albino is derived from Latin "albus", which means white. It is usually used to describe the individual of albinism. However, some people may consider the term offensive because it emphasizes their condition over their individuality. Therefore, it is generally preferred to refer to someone as 'a person with albinism' rather than an 'albino. Is Albinism a disease? It is important to note that albinism is not a disease. It is a genetic disorder that a person is born with. While this is a lifelong condition that cannot be cured or grown with proper care and management strategies, individuals with albinism can lead to a healthy life. What are the different types of Albinism? Albinism types are distinguished by the extent and distribution of melanin deficiency: Oculocutaneous Albinism (OCA): This condition affects the skin, hair, and eyes, causing varying degrees of pigment loss. Its subtypes include OCA1, OCA2, OCA3, and OCA4, each caused by mutations in a different gene. Ocular Albinism (OA): Primarily affects the eyes, leading to vision problems due to an abnormal development of the retina and optic nerve. In which skin and hair may have minimal to no pigment changes. Hermansky-Pudlak Syndrome (HPS): This condition is characterized by a partial albinism with bleeding disorders and in some cases, lung and bowel complications. It results from mutations affecting lysosome-related organelles. Chediak-Higashi Syndrome: It is a rare and severe form characterized by partial albinism, recurrent infections and neurological abnormalities due to a genetic defect affecting lysosomal trafficking. Griscelli Syndrome: This condition presents silver-gray hair, partial albinism, and immune system abnormalities that include immunodeficiency and hemophagocytic lymphohistiocytosis. Understanding these albinism types helps in diagnosing and managing albinism-related conditions, focusing on addressing associated health issues and providing necessary support for affected individuals. What causes Albinism? Albinism causes an absence of melanin in the skin, hair and eyes due to a genetic mutation. These mutations disrupt the production or distribution of melanin, leading to the characteristic features of albinism. What are the symptoms of Albinism? Albinism symptoms are mainly visible in human skin, hair and eyes. However, differences can sometimes be slight. Here are some key symptoms: Skin Pale skin color compared to siblings or blood relatives Sensitivity to sun exposure leading to freckles or moles Lack of ability to tan Hair Hair color can range from very white to brown Eye Color Eyelashes and eyebrows are often pale Eye color can range from very light blue to brown Vision Rapid, uncontrollable movement of the eyes (Nystagmus) Extreme sensitivity to light (Photophobia) Poor depth perception Legal blindness in severe cases If you notice any of these signs in your child, it's crucial to consult with your healthcare provider. How is Albinism diagnosed? When a child is born with the lighter skin and the color of the hair of the expected, this may alert healthcare providers to the possibility of albinism. They will probably order an eye exam and monitor any changes in the color and vision of the child's skin for a definitive diagnosis. Also, if your child with albinism experiences frequent nosebleeds, easy bruising or long-term infections, it is important to contact your healthcare provider immediately. These symptoms may suggest rare but serious hereditary conditions that include albinism. What is the treatment for Albinism? Although there is no cure for albinism, people with the disorder can lead fulfilling lives by taking steps to protect their skin and eyes and get appropriate care. Here are some albinism treatment strategies: Sun Protection: Protecting the skin from sun exposure is important to prevent sunburn and skin cancer. This can be achieved by wearing protective clothing, applying sunscreen and avoiding the midday sun. Vision Care: Regular visits to an eye specialist can help manage the vision problems associated with albinism. Treatments includes prescription glasses, contact lenses, and vision aids. Regular Skin Checks: As people with albinism are at a higher risk for skin cancer, regular skin exams are essential for early detection and treatment. Support and Counseling: Due to distinctive appearance, people with albinism may face social and emotional challenges. Support groups, counselling, and educational programs can be beneficial in such cases. Can Albinism be prevented? Since albinism is an inherited condition, it cannot be prevented. However, if you have a family history of albinism, you can consult a genetic counsellor who can explain the chances of having a future child with albinism symptoms and can also discuss available genetic tests. What complications can occur because of Albinism? People with albinism may face some complications related to vision challenges and increased sensitivity to sunlight. They may also experience social and emotional problems due to their unique appearance. It is important to address these issues with the right care and support. What is the outlook for Albinism? Although there is no cure for forms of albinism, most people with the condition lead normal lives with the same lifespan as anyone else. However, they may face challenges such as sun sensitivity and vision impairments, which can be managed with the right strategies. When to see a doctor? If you notice signs of albinism in your child, or if albinism runs in your family, it is recommended that you speak to your doctor or a genetic counselor who can provide accurate information, support and advice about the condition. Conclusion Understanding the causes, symptoms, types, and treatment strategies for albinism can empower you or your loved ones dealing with this condition to lead fulfilling lives. Remember that each person's journey with albinism is unique therefore personalized medical advice is essential. Metropolis Healthcare offers advanced diagnostic services right at your doorstep; their qualified technicians collect samples at your home for processing in their state-of-the-art labs. Test results are shared online, making them readily accessible. They are committed to providing reliable, personalized care to empower patients in prioritizing their health.
Boils and Carbuncles: Symptoms, Causes, and Effective Treatment Methods
What are Boils and Carbuncles? A boil is a painful, pus-filled bump that forms under the skin due to a bacterial infection in one or more hair follicles. Initially begins as a tender reddish or purplish bump, it quickly fills with pus becoming larger and more painful until it ruptures and drains. On the other hand, a carbuncle is a cluster of boils creating an interconnected area of infection beneath the skin. They cause deeper infections compared to single boils and often leave scars. What are the symptoms of a Boil? Boil symptoms typically include: Red, Painful Bump: The initial sign is a small, firm, red, and tender bump on the skin Swelling: The area around the boil becomes swollen and inflamed Pus Formation: The center of the boil fills with pus, creating a white or yellow tip Warmth: The skin around the boil feels warm to the touch Increased Size: The boil gradually enlarges as it fills with more pus Swollen Lymph Nodes: Nearby lymph nodes may become swollen and tender What are the symptoms of Carbuncles? Carbuncle symptoms include: Multiple Painful, Red Bumps: Typically larger and deeper than single boils Swelling: The surrounding skin becomes swollen and tender Pus Drainage: Multiple heads may release pus Fever and Chills: Systemic symptoms like fever and chills can occur Fatigue: General feeling of malaise What causes Boils and Carbuncles? Most boils are caused by Staphylococcus aureus, a type of bacteria which is commonly found on the skin and inside the nose. The bacteria causes a bump to form as pus collects under the skin. Boils causes often include sites where the skin has been broken by a small injury or an insect bite, giving the bacteria easy entry. Certain factors increase your risk of developing these conditions including a close contact with someone who has a staph infection, diabetes or other skin conditions like acne and eczema that damage your skin's protective barrier, and compromised immunity. Can I treat a Boil at home? A boil treatment at home can often be effective, especially for smaller boils that haven't progressed too far. Here are some steps you can take: Firstly, applying hot compresses to the boil several times a day. This encourages the growth of the boil and encourages its natural drainage. Use a clean washcloth dipped in warm water and keep it boiling for about 10 to 15 minutes at a time. Next, once the boil starts to drain, keep the area clean and covered with a sterile bandage. This prevents the spread of infection and helps the healing process. You can also try over-the-counter treatments like topical antibacterial ointments, which can help to prevent infection and promote healing. Make sure to follow the instructions on the package and consult a pharmacist if you have any questions. It's important not to try to squeeze or "pop" the boils and carbuncles yourself, as this can spread the infection or lead to further complications. If the boil is large, very painful, or doesn't improve with home treatment, it's best to seek medical attention. A healthcare provider may need to drain the boil and, in some cases, prescribe antibiotics to treat the infection. By taking these steps, you can often effectively manage boils and carbuncles at home and promote quicker healing. How can I prevent a Boil or Carbuncle? Preventing boils and carbuncles can be challenging for those with weakened immune systems. Here are some measures that might help avoid staph infections: Regular hand washing with mild soap or using an alcohol-based hand rub Avoid close contact with someone who has a staph infection, boil or carbuncle Keeping wounds clean and covered until they heal Avoid sharing personal items like towels, clothing or razors What is the outlook for people with Boils and Carbuncles? The outlook for people with boils and carbuncles is generally good with proper treatment. Most boils and smaller boils can be treated effectively at home with warm compresses, good hygiene, and sometimes topical antibiotics. They typically heal within a few weeks, although larger or more severe cases may require medical intervention such as drainage or taking oral antibiotics. What are the complications of Boils and Carbuncles? Complications can arise if the infection spreads or recurs, especially in individuals with a compromised immune systems or chronic medical conditions. In rare cases, bacteria from boils or carbuncles can enter your bloodstream and travel to other body parts leading to deep infections like sepsis, endocarditis, and osteomyelitis. Seeking medical advice promptly is advisable if boils are recurrent, large, very painful, or accompanied by fever. With appropriate treatment, the majority of people can recover fully without long-term consequences. How can I keep my Carbuncles from spreading to others? To prevent your carbuncles from spreading to others: Avoid skin-to-skin contact until your carbuncle completely heals Wash your clothes, bedding, and towels regularly Cover the carbuncle with a bandage Use antibacterial soap, especially if you have been exposed to a carbuncle. Do not squeeze or puncture the head of the carbuncle. Carefully wrap dressings and bandages covering the carbuncle and discard. Conclusion Treating boils and carbuncles can be uncomfortable and painful. But understanding its causes and symptoms is the first step to effective treatment. Good hygiene is necessary to prevent these conditions. Remember to consult a healthcare provider for an accurate diagnosis and treatment. At Metropolis Healthcare, we are committed delivering reliable results and personalized care for all our patients. Our qualified technicians make at-home visits for blood sample collection which is processed at our advanced labs. Test reports are conveniently shared online via email or through our Metropolis TruHealth app. Prioritize your health today with our trusted services.
Understanding Broken Collarbone (Clavicle Fracture): Symptoms, Types, and Treatment
What is a Broken Collarbone (Clavicle Fracture)? A broken collarbone or clavicle fracture occurs when the clavicle bone, connecting the shoulder to the sternum, is cracked or broken. It's often caused by falls, sports injuries or accidents. Symptoms include pain, swelling and difficulty moving the arm. Treatment usually includes immobilization, pain management and sometimes surgery. What are the types of Clavicle Fractures? Clavicle fracture types are typically classified on their location: Midshaft Fractures: These fractures occur in the middle third of the clavicle and are the most common type, often resulting from direct trauma or falls. Distal (Lateral) Fractures: These fractures occur near the shoulder joint and are less common. They may be more complex due to the possible involvement of ligaments and acromioclavicular joints. Medial (Proximal) Fractures: These fractures are rare and occur near the sternum. They often require careful assessment of injuries associated with adjacent structures such as the chest or lungs. Each clavicle fracture type varies in severity and treatment approach. How common are Clavicle Fractures? The frequency of clavicle fractures is highest during adolescence and decreases after the age of 20. However, in older adults this frequency increases again due to the weakening of bone strength with age. What are the symptoms of a Broken Collarbone? A broken collarbone, or clavicle fracture, is revealed through several distinct symptoms, which are primarily localized around the shoulder and upper chest area. Common clavicle fracture symptom includes severe pain at the fracture site, often exacerbated by shoulder movement. The pain is usually immediate and severe, making it difficult to move the affected arm or shoulder. Swelling and tenderness around the collarbone are typical, with visible bruising or a bump over the break area as the blood vessels and soft tissues around the fracture are affected. In some cases, the broken ends of the bone may protrude against the skin, creating a noticeable deformity or even breaking through the skin in severe cases. A grinding or clicking sensation may be felt when attempting to move the shoulder, indicating bone fragments rubbing against each other. The affected arm may also appear shorter because the shoulder is collapsed inward toward the chest. Additionally, clavicle fracture symptoms could include numbness or tingling in the shoulder and arm, indicating potential nerve involvement. Decreased mobility is common, as pain and mechanical disturbance prevent normal movement of the shoulder. In case if the injury is severe, there may be associated injuries to nearby structures, such as the lungs or major blood vessels, which can cause additional collarbone fracture symptoms like shortness of breath or a feeling of chest tightness. What are the causes of Clavicle Fractures? Now that we have explored the symptoms, let's look at clavicle fracture causes. Some of the common causes include: Falls: Landing directly on your shoulder or onto an outstretched arm Sports injuries: A direct blow to the shoulder while playing a sport Traffic accidents: Accidents involving cars, motorcycles, or bicycles Birth injury: Infants sometimes suffer clavicle fractures during difficult vaginal births How is a Broken Collarbone diagnosed? If you show clavicle fracture symptoms, your doctor will examine the area and likely order an X-ray. Imaging tests can provide detailed views of dense structures, like bones, and will help your doctor determine the type and severity of the clavicle fracture. How is a Broken Collarbone treated? Treatment options for a broken collarbone or clavicle fracture depends on the fracture's severity, location, and alignment. Most clavicle fractures can be treated non-surgically, while more severe cases may require surgical intervention. Non-Surgical Clavicle Fracture Treatment For less severe fractures, especially those where the bone fragments remain aligned, non-surgical treatment is often effective. This involves: Immobilization: Using a sling or figure-of-eight bandage to immobilize the arm and shoulder to allow the bones to heal. It is usually worn for several weeks. Pain Management: Using over-the-counter pain relievers, such as ibuprofen or acetaminophen, are effective for managing discomfort and alleviating inflammation. Ice Application: Applying ice packs to the injured area helps reduce swelling and pain. Physical Therapy: Once the initial healing phase is over, physical therapy exercises are introduced to restore shoulder strength and range of motion. Surgical Clavicle Fracture Treatment Surgery may be necessary for more severe fractures, especially if the bone fragments are significantly displaced or if the fracture has broken through the skin. Surgical options include: Open Reduction and Internal Fixation (ORIF): This procedure involves moving the bone fragments and fixing them with plates, screws, or pins to ensure proper alignment and healing. Post-Surgical Care: After surgery, a period of immobilization is followed by physical therapy to regain shoulder function and strength. Recovery time for a broken collarbone varies from person to person, but most patients can resume normal activities within a few months. Regular follow-up appointments with a healthcare provider ensure proper healing and address any complications that may arise. What happens if a Broken Collarbone Goes Untreated? If left untreated, a broken collarbone can lead to complications such as: Nerve or Blood Vessel Injury Poor or Slow Healing Shortening of the bone due to improper healing Increased risk of Osteoarthritis in the affected joint How Long Does it Take to Recover from a Broken Collarbone? Recovery from a broken collarbone varies by age: adults typically heal in 8-12 weeks, adolescents in 6-8 weeks, children under 8 in 3-6 weeks, and infants in about 2 weeks. Your healthcare provider will advise when you can resume normal activities. Will a Broken Collarbone Cause Any Long-Term Complications? With proper clavicle fracture treatment, long-term complications are rare. However, some people may develop lumps over the bones, which usually subside over time. What Should I Do and Not Do with a Broken Collarbone? Healing a broken collarbone requires patience and following doctor's recommendations. Do's: Use a sling and immobilizer as advised Take prescribed medications Attend physical therapy sessions Don'ts: Avoid moving the injured arm without medical advice Do not lift heavy objects Avoid activities that could lead to another fall When to see a doctor? If you experience persistent pain in your collarbone region, it is important to seek medical attention immediately. Seeing a doctor immediately can help to prevent complications associated with untreated clavicle fractures. Conclusion A broken collarbone might be painful and uncomfortable, but with early diagnosis, effective collarbone fracture treatment, and careful rehabilitation, a full recovery is the norm. While, prioritizing your health and don't ignore discomfort or possible symptoms. Remember, with accurate knowledge and professional medical care, your health is within your reach. For reliable diagnostic services, consider Metropolis Healthcare. Our advanced diagnostic labs offer accurate pathology testing services right at your doorstep. Results are made available online for easy access. Trust us for personalized care dedicated to empowering you to prioritize your health.
Exploring Broken Heart Syndrome
What is Broken Heart Syndrome? Broken heart syndrome, or Takotsubo cardiomyopathy, is a temporary heart condition often triggered by intense physical or emotional stress. The term "broken" refers to the fact that a person's heart may suddenly manifest symptoms similar to a heart attack, such as chest pain or shortness of breath, even if their coronary arteries are unobstructed. In extreme cases, this disease can be life-threatening. Types of Broken Heart Syndrome Broken heart syndrome comes in four distinct types. The most common type is apical, accounting for over 80% of cases, and affects the lower half of the heart, causing it to balloon outward. Mid-ventricular broken heart syndrome impacts the middle section of the heart’s lower chambers (ventricles), creating a belt-like appearance around the heart. In this type, the upper and lower sections function normally. Basal broken heart syndrome, is a rare condition that accounts for about 2% of cases and affects the upper area of the heart, which resembles a belt or ring, leaving only the lower part to function normally. Focal, this rarest form, accounts for about 1% of cases and affects a smaller, localized area. This type forms a noticeable bulge that protrudes from the heart, while the opposite side curves inward. Understanding these types aids in accurate diagnosis and targeted treatment for those affected by this unique cardiomyopathy. How Common is Broken Heart Syndrome? Though the exact numbers are tricky to determine due to misdiagnosis as a heart attack, studies show that about 2 % of people who present the symptoms of a heart attack may actually have broken heart syndrome. Especially postmenopausal women are more likely to experience this condition than men. What are the Symptoms of Broken Heart Syndrome? Broken heart syndrome symptoms often mimic those of a heart attack. Common signs include sudden chest pain, shortness of breath, and irregular heartbeat. Other symptoms may include sweating, dizziness, and fainting. Unlike a heart attack, broken heart syndrome is typically triggered by severe emotional or physical stress rather than blocked coronary arteries. Immediate medical attention is crucial for proper diagnosis and treatment to manage these symptoms effectively. Broken Heart Syndrome vs. Heart Attack Broken heart syndrome mimics heart attack symptoms like chest pain and shortness of breath but differs as it is triggered by emotional or physical stress, and not because of blocked arteries. Heart attacks involve artery blockages leading to heart muscle damage, while in most cases, broken heart syndrome causes temporary heart function disruption. What Causes Broken Heart Syndrome? While the exact broken heart syndrome causes remain unknown, it is often triggered by severe stress. The heart's reaction to a surge of stress hormones causes temporary heart muscle failure. Triggers can range from the death of a loved one, divorce, surprise parties, physical stressors like an asthma attack or surgery, and even intense fear or anxiety. What Kinds of Emotional and Physical Stress Can Cause Broken Heart Syndrome? Emotional stressors may include: Grief at the death of a loved one Divorce breakup Domestic abuse Intense fear anxiety Physical stressors may include: Surgery Asthma Attack Severe Infection Drug Abuse What Are the Risk Factors for Broken Heart Syndrome? Though anyone can get it, broken heart syndrome risk factors include: Being Female: Post-menopausal women are at higher risk Age: It is more common in people aged over 50 History of Neurological Conditions or Mental Health Disorders: Individuals with conditions such as epilepsy or anxiety disorders are at greater risk. What Are the Complications of Broken Heart Syndrome? Complications of broken heart syndrome include heart failure, arrhythmias (irregular heartbeat), and blood clots. In severe cases, it can lead to cardiac shock, when the heart is suddenly can't pump enough blood. Although these complications are rare, they emphasize the importance of prompt medical attention and monitoring. How is Broken Heart Syndrome Diagnosed? Diagnosis of broken heart syndrome usually occurs in an emergency situation because the symptoms are similar to those of a heart attack. A health care professional will examine you and ask about your symptoms and medical history. Tests which help to diagnose broken heart syndrome includes Blood Tests, Electrocardiogram (ECG), Coronary Angiogram, Echocardiogram, and Cardiac MRI. What is the Treatment for Broken Heart Syndrome? Once diagnosed, broken heart syndrome treatment focuses on relieving symptoms using medicines like ACE Inhibitors, ARBs, Beta Blockers, Diuretics, and Blood Thinners if there is a clot present. How can Broken Heart Syndrome be Prevented? Preventing broken heart syndrome involves managing stress and maintaining a healthy lifestyle. Engage in regular physical activity, practice relaxation techniques such as meditation and yoga, and get enough sleep. Building a strong support network of family and friends can also help reduce emotional stress. Avoid excessive alcohol and tobacco use, as these can increase stress levels. If you experience high stress or emotional trauma, seek professional counselling or therapy to develop effective coping strategies and reduce the risk of developing broken heart syndrome. What Can I Expect If I Have Broken Heart Syndrome? If you have broken heart syndrome, you can expect sudden chest pain and shortness of breath, often triggered by stress. Unlike a heart attack, it is usually temporary, with most people recovering fully within weeks. Treatment focuses on managing symptoms and stress, with follow-up care to monitor heart health. What Is the Outlook for Broken Heart Syndrome? Though it can be severe or even life-threatening in the immediate phase, most people survive and recover fully from broken heart syndrome. However, recurrence is possible in about 10% of cases. Is Broken Heart Syndrome Serious? Yes. While it is typically reversible with proper care and management, severe cases can lead to serious complications such as congestive heart failure or even death. Conclusion Understanding broken heart syndrome is vital for recognizing its symptoms and seeking timely medical attention. Metropolis Healthcare's expert pathology services can assist in diagnosing this condition with their at-home blood testing and health check-ups, making it easier for you to prioritize your heart health. Remember, informed and proactive health decisions can make a world of difference when it comes to safeguarding your heart.
Intermittent Fasting: Benefits, Schedule, and Side Effects
What is intermittent fasting? Intermittent fasting (IF) is a dieting method that alternates periods of fasting and eating. Unlike traditional diets which focus on what you eat, intermittent fasting focuses on when you eat. Common methods include the 16:8 method, where you fast for 16 hours and eat within an 8-hour window, and the 5:2 method, where you eat normally for five days and then drastically reduce your calorie intake for two consecutive days. The primary goal of intermittent fasting is to allow the body to use stored fat for energy during fasting periods, which can aid in weight loss and improve metabolic health. In addition, intermittent fasting has been linked to benefits such as improved insulin sensitivity, reduced inflammation, and improved brain health. However, it may not be suitable for everyone and it is important to consult a healthcare professional before starting intermittent fasting, especially for people with underlying health conditions. What are the types of intermittent fasting? Intermittent fasting encompasses several popular methods, each varying in the duration and frequency of fasting periods. The 16/8 method involves fasting for 16 hours and eating within an 8-hour window daily. Another approach, the 5:2 diet, It involves eating normally five days a week and fasting two days a week, with a calorie limit of 500-600 on those days. Alternate-day fasting alternates between normal eating and fasting days. Additionally, the Eat-Stop-Eat method involves fasting for 24 hours once or twice a week. These diverse methods cater to different lifestyles and goals, and promotes weight loss, improved metabolic health, and other potential health benefits. How does intermittent fasting work? When we eat, our body spends a few hours processing the food and absorbing nutrients. During this process, our body is in a 'fed state' where it's difficult to burn fat due to high insulin levels. In contrast, when we avoid eating, our insulin levels drops and it encourage fat burning this is the 'fasted state'. By following an intermittent fasting schedule, we cycle between the fed and fasted state which potentially aids weight loss and provides other health benefits. Intermittent fasting benefits Intermittent fasting is more than just a fancy diet. It's an effective lifestyle change with several potential benefits: Promotes Weight Loss: Limiting eating window through intermittent fasting for weight loss can assist lower calorie intake and speed up metabolism. Improves Insulin Sensitivity: Intermittent fasting enhances your body's reaction to insulin, which can aid with blood sugar management. Encourages Cellular Repair: Periods of fasting can trigger autophagy, where your body cleanses itself of damaged cells, promoting longevity. Boosts Heart Health: Intermittent fasting may improve various risk factors for heart disease such as blood pressure and cholesterol levels. Enhances Brain Function: Some studies suggests that intermittent fasting may boost neuroprotection and improve cognitive functions. In this way, intermittent fasting benefits not just your weight loss journey but also contributes holistically to your health. Who should be careful or avoid it? Although intermittent fasting is beneficial for most people, some groups should be cautious or avoid it altogether. These includes pregnant women, breastfeeding mothers, those with diabetes or kidney stones, etc. Always consult a healthcare professional before starting any new dietary regimen. When does intermittent fasting work best? To make intermittent fasting more effective, it is crucial to personalise the approach based on the lifestyle and individual preferences. Start by choosing a fasting method that aligns with daily routines and eating habits. Try different fasting periods, like the popular 16/8 method or alternate-day fasting, to find what's sustainable and manageable for you. Plan your meals around during your eating windows to ensure a balanced diet and proper hydration. Begin fasting gradually, starting with shorter fasting periods if necessary, to give your body a chance to adapt. Monitor energy levels, hunger cues and general health to adjust fasting plans as needed. Consistency is key. Stick to your chosen intermittent fasting schedule to gain potential benefits over time, such as weight management and improved metabolic health. Should females fast? Women can also gain huge intermittent fasting benefits, but they need to be cautious as drastic changes in meal timings can affect their menstrual cycle. Hence, females should start with lighter fasting schedules and monitor their body's reactions. Is intermittent fasting safe? Yes, intermittent fasting is generally safe for healthy individuals. However, it's vital to listen to your body and adjust your fasting schedule if needed. What are the side effects of intermittent fasting? Along with its appealing benefits, intermittent fasting side effects could range from hunger pangs, fatigue, insomnia, nausea or headaches initially as your body is adjusting to the new eating pattern. Frequently Asked Questions Can I drink liquids during the fast? Yes, water, black coffee or tea without sugar or cream can be consumed during fasting periods. Isn’t it unhealthy to skip breakfast? Not necessarily! The idea is not about skipping meals, but changing when you eat them. So, if you follow a time-restricted diet, like 16: 8, where you skip breakfast but ensure the intake of nutrients during the food window, it is perfectly healthy. Can I take supplements while fasting? You can continue to take most supplements during fasting. However, some fat-soluble vitamins are better absorbed with food. Can I work out while fasting? Yes! As working out in a fasted state utilizes fats for providing energy, promoting weight loss. Will fasting cause muscle loss? No, research shows that fasting promotes fat loss while preserving muscle mass. However, maintaining a good protein intake and regular strength training can help prevent muscle loss. Conclusion Overall, intermittent fasting is a dietary approach with potential health benefits ranging from weight management to improved metabolic health. Although it is not a one-size-fits-all solution, with proper planning and precautions it can be an effective lifestyle change. At Metropolis Healthcare, we believe in empowering you to prioritise your health through reliable diagnostics services. Make informed healthcare decisions with our comprehensive health check-ups and blood tests at home service. Take charge of your health today with Metropolis!
 Home Visit
Home Visit Upload
Upload




















 WhatsApp
WhatsApp