Latest Blogs
Ascites: Causes, Symptoms, and Treatments
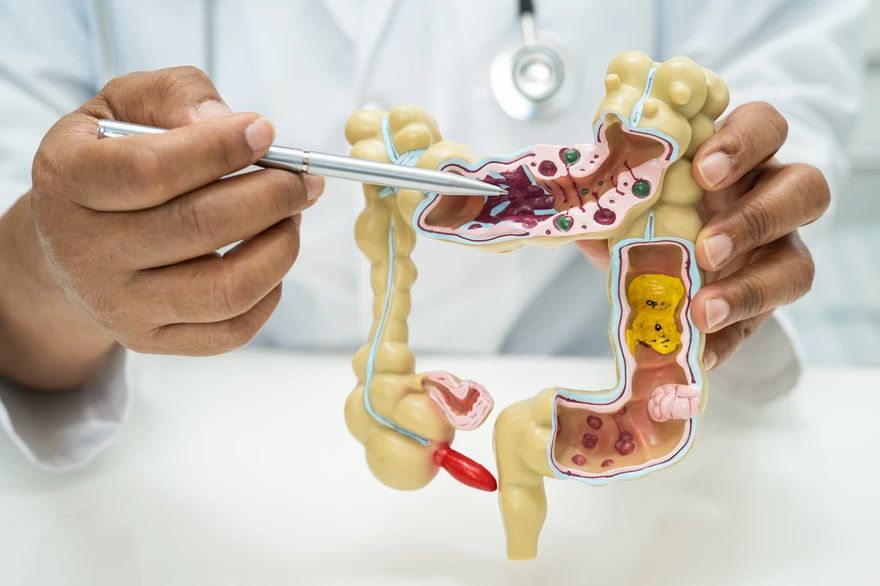
What is Ascites? Ascites is a medical condition characterised by the abnormal accumulation of fluid in the abdominal cavity, specifically between the layers of the peritoneum. This condition often results from liver diseases, particularly cirrhosis, but can also be caused by heart failure, cancer, or infections. As fluid builds up, it can lead to abdominal swelling and discomfort, impacting daily activities. Ascites symptoms may include a feeling of fullness, nausea, and shortness of breath due to pressure on the diaphragm. Effective management involves addressing the underlying causes and may include dietary changes and medications. Understanding ascites is crucial for prevention and treatment strategies. How Common is Ascites? Before getting too concerned about ascites, it’s important to know that this condition typically doesn’t affect healthy individuals. However, it is not uncommon among those with liver-related diseases such as cirrhosis. In fact, ascites is common complication of cirrhosis, affecting about half of people with decompensated cirrhosis. But don't let this statistic frighten you; instead, let's understand the risk factors, symptoms, and potential ascites treatments. What are the Risk Factors for Ascites? The main risk factor for developing ascites is having a condition that leads to cirrhosis of the liver. These conditions include non-alcohol-associated fatty liver disease, hepatitis B and C, alcohol use disorder, and genetic liver diseases such as hemochromatosis. Other factors that can contribute to ascites include congestive heart failure, kidney failure, and certain types of cancer. What Causes Ascites? The most common cause of ascites is liver cirrhosis, often resulting from an excessive alcohol consumption. However, ascites causes can also include advanced or recurrent cancers, heart conditions, dialysis, low protein levels, and infections. Cirrhosis, the primary cause of ascites, affects liver function, when combined with portal hypertension (high pressure in the portal vein that supplies blood to the liver), leads to symptoms associated with ascites. This increased pressure forces fluid to leak from the veins and accumulate in the abdominal cavity. How does Cirrhosis cause Ascites? Cirrhosis causes ascites primarily through the development of portal hypertension, which is increased pressure in the blood vessels surrounding the liver. As liver function worsens, blood flow becomes obstructed, causing a fluid accumulation in the abdominal cavity. Furthermore, cirrhosis also affects kidney function, making it harder for the kidneys to eliminate excess salt and fluid. This combination of factors results in ascites, which can greatly affect a patient's quality of life and indicate advanced liver disease. What are the Symptoms of Ascites? The main ascites symptoms are a large belly and rapid weight gain. Other symptoms can include: Swelling in your ankles Shortness of breath Digestive issues such as bloating, abdominal pain, loss of appetite or constipation Back pain Difficulty sitting due to abdominal discomfort Fatigue How is Ascites Diagnosed? Ascites is diagnosed through a physical examination, along with an assessment of your symptoms and medical history. The healthcare provider might perform a procedure to extract fluid from your abdomen with a needle for testing. Which can help in detecting conditions like cancer or infection. Additionally, they may order imaging tests such as ultrasound, MRI, or CT scans to get a clearer view of your abdomen. What Tests Might I Need? After the initial examination, the healthcare provider may recommend further tests to help help identify ascites causes. These include: Ultrasound or CT Scan: These imaging scans provide a detailed view of the abdominal area. Paracentesis: Here, a needle is inserted into your abdomen to remove fluid which is then analysed for signs of cancer, infection or other conditions. How is Ascites Treated for Ascites? Ascites treatment usually begins with lifestyle changes, like limiting salt and fluid intake and avoiding alcohol consumption. Doctors may prescribe diuretic medicines to help the body get rid of excess fluid. In some severe cases, large amounts of fluid might need to be drawn from your abdomen through a needle. Complex cases might require procedure called Transjugular Intrahepatic Portosystemic Shunt (TIPS), where a connection is made inside the liver between blood vessels to alleviate high pressure causing ascites. Will I Need Surgery for Ascites? Surgery might be necessary for ascites if less invasive treatments, such as diuretics or dietary changes are ineffective. Common surgical options include paracentesis, where fluid is removed from the abdomen, and transjugular intrahepatic portosystemic shunt (TIPS), which helps reduce portal hypertension by creating a pathway for blood flow. In severe cases, a liver transplant might be required if liver function is compromised. Early intervention is crucial, as effective ascites treatment can prevent complications and improve quality of life. Regular monitoring and management strategies are necessary to see if surgery is needed, ensuring patients receive appropriate ascites treatment based on their specific condition and response to initial therapies. What Other Treatments are Available for Ascites? When is the underlying cancer causes ascites, treatments like chemotherapy or hormone therapy can help shrink the tumor and stop fluid accumulation. Since every patient's case is unique, it's important to personalise the treatment based on individual medical advice. Can Ascites Be Cured? While ascites may not be completely curable, its symptoms can be effectively managed with appropriate treatment. In some patients, diuretic therapy, procedures like TIPS, or a liver transplant can help resolve ascites. How Can I Prevent Ascites? The best way to prevent ascites is by leading a healthy lifestyle. Limiting alcohol and salt intake, avoiding smoking, maintaining a healthy weight and exercising regularly. How Can I Control Ascites? There are several strategies to help manage ascites: Limit Salt Intake: Reducing sodium is essential to minimize fluid retention, so a low-sodium diet is important. Use Diuretics: Doctors may prescribe diuretics to help remove excess fluid from the body. Restrict Fluid Intake: It's also important to limit fluid intake and avoid alcohol, as it can worsen liver function. Monitor Weight: Keeping an eye on your weight can help track fluid accumulation, allowing for quick action if significant changes occur. Paracentesis: In some cases, a procedure called paracentesis may be needed to drain large amounts of fluid. Overall, effective ascites treatment focuses on managing the underlying conditions and making lifestyle changes to improve symptoms and prevent complications. What’s the Outlook for People with Ascites? Ascites indicates impaired liver function, which requires prompt medical attention. With appropriate treatments and lifestyle modifications, you can manage ascites effectively. What are Complications of Ascites? Ascites complications can greatly affect a patient's health and overall quality of life. One of the most serious ascites complications is spontaneous bacterial peritonitis (SBP), an infection that occurs when bacteria proliferate in the ascitic fluid, leading to severe abdominal pain and fever. Other complications can include kidney failure from increased pressure on the renal blood vessels, and umbilical hernias, where abdominal organs protrude through the weakened areas in the abdominal wall due to fluid accumulation. Furthermore, ascites can lead to difficulty breathing as the fluid accumulates in the abdomen and exerts pressure on the diaphragm. These complications highlight why it's important to manage and treat ascites effectively. Quick action can prevent the patient's condition from getting worse. Both patients and healthcare providers need to understand these ascites complications to ensure proper monitoring and care. Is Ascites Life Threatening? Ascites can be very life-threatening because of potential complications. One major risk is spontaneous bacterial peritonitis, an infection that can happen in the accumulated fluid. If untreated, this infection can lead to sepsis and organ failure. Other ascites complications includes kidney failure and malnutrition, which can worsen health problems. While ascites itself may not be directly life-threatening, it often indicates serious underlying issues, like liver disease, that need urgent medical attention to avoid serious consequences. Can Ascites Come Back? Yes, the fluid can keep building up, so ongoing management is essential. If the fluid returns quickly, further treatments may be needed. If I have Ascites, How can I Best Take Care of Myself? Consulting a dietitian for a sodium-restricted diet plan, regular weight monitoring, avoiding alcohol, and managing any underlying conditions like Hepatitis B or C. When Should I Consult my Doctor? If you experience a fever, stomach pain, or see a sudden weight gain, treat it as a warning sign that requires immediate medical attention. Conclusion Ascites may feel overwhelming initially, but understanding its causes, symptoms, and treatment strategies can help you manage this condition effectively. Make sure to take care of your health by consulting a doctor and getting the right guidance. For reliable diagnostic services and health check-ups from the comfort of your home, consider Metropolis Healthcare. Their advanced labs provide accurate testing facilities and their team of qualified technicians offers at-home blood sample collection services. Empower yourself today by taking control of your health with Metropolis Healthcare.
Ascariasis: Causes, Symptoms, and Treatment Options
What is Ascariasis? Ascariasis is a parasitic infection caused by the roundworm Ascaris lumbricoides. It is one of the most common human worm infections, affecting over 760 million people worldwide, primarily in tropical and subtropical regions with poor sanitation. This infection occurs when individuals consume food or water tainted with Ascaris eggs from feces. The eggs hatch in the intestines, and the larvae migrate through the body, causing various symptoms depending on their location. In the lungs, the larvae can cause pneumonia-like symptoms, including cough, wheezing, and difficulty breathing. In the intestines, ascariasis may result in abdominal pain, nausea, vomiting, diarrhoea, and malnutrition, particularly in children. In severe cases, a significant number of worms can result in intestinal blockage, which is a serious medical emergency. Ascaris treatment involves using antiparasitic medications, while prevention emphasises better sanitation, handwashing, and safe food handling. Although most cases are mild or have no symptoms, heavy infestations can result in serious complications, highlighting the importance for early diagnosis and treatment. What are the Types of Ascariasis? It may be surprising, but there are different types of ascariasis exist. The most common is caused by the human roundworm (Ascaris lumbricoides), which is responsible for most cases. Another type is the pig roundworm (Ascaris suum). Although rarer, this type can also cause human infections, particularly in those who raise pigs or use pig manure for fertilisation. How Common is Ascariasis? Ascariasis affects more than 1 billion people globally, making it one of the most common parasitic infections and the most widespread type of intestinal worm infection. Children in tropical and subtropical regions with poor sanitation are especially at risk. The infection occurs when people accidentally ingest Ascaris eggs through contaminated food or water, causing symptoms like stomach pain, nausea, and malnutrition. Enhancing sanitation and hygiene practices can significantly reduce the risk of this infection. What are the Symptoms of Ascariasis? Ascaris symptoms can be misleading, as most of the people are affected may have a few or no noticeable symptoms. However, there are some medical practitioners can detect the underlying symptoms. Infection in Your Lungs When Ascaris lumbricoides larvae migrate through the lungs, they can cause respiratory symptoms similar to asthma or pneumonia. Its common signs includes persistent cough, wheezing, and shortness of breath. Some individuals may also experience fever and, in rare cases, blood in their sputum. These symptoms typically arise about 10 to 14 days after infection as the larvae travel from the intestines to the lungs. Infection in Your Intestines In the intestines, ascariasis can cause different gastrointestinal symptoms. Mild infections might show up as uncertain abdominal pain and nausea, while more severe infections can lead to vomiting, diarrhea, and even blood in the stool. Heavier infections can lead to intestinal blockages, resulting in intense abdominal cramps and possible malnutrition, especially in children. In extreme cases, adult worms may be expelled in vomit or stool, which can be quite distressing. Recognising these symptoms early is crucial for effective treatment and management of ascariasis. What Causes an Ascariasis Infection? Ascariasis is caused by swallowing the eggs of the human roundworm A. lumbricoides. Once ingested, these parasites thrive throughout the human body, wherein they mature and reproduce. This leads to various health issues, particularly affecting those with poor sanitation and hygiene practices. How is Ascariasis Transmitted? Unlike some diseases that spread directly from person to person, ascariasis follows a different path. Transmission occurs when a person comes into contact with soil mixed with infected human or pig faeces or contaminated water. The microscopic eggs present in these mediums can get into our bodies when we swallow them. This can happen through hand-to-mouth contact or by consuming uncooked fruits or vegetables grown in contaminated soil. Notably, children are more prone to this infection due to their increased likelihood of playing in dirt and putting their dirty fingers into their mouths. Hence it's essential to maintain good hygiene practices and ensure children understand the importance too. What is the Life Cycle of A. lumbricoides? Understanding the life cycle of the Ascaris lumbricoides roundworm can shed light on how ascariasis spreads: Ingestion: The tiny ascariasis eggs cannot become infective without coming into contact with soil. People unknowingly ingest these eggs through dirty hands or by eating uncooked fruits or vegetables grown in contaminated soil. Migration: After hatching in your small intestine, the larvae migrate to your heart and lungs via your bloodstream or lymphatic system. They mature in your lungs over 10-14 days before making their way back to your intestines via your throat. Maturation: Once back in the intestines, the parasites grow into adult worms. Reproduction: Female worms can produce up to 200,000 eggs a day which exit your body through feces and become infective once they contact soil. This entire process takes approximately two to three months. Who is at Risk for Ascariasis? Certain factors increase the risk of contracting ascariasis. Age: Children aged 10 and younger are most susceptible, as they are more likely to play in contaminated soil and put their fingers in their mouths. Climate: Ascariasis is more prevalent in warm, tropical, and subtropical regions with poor sanitation. Sanitation: Lack of access to clean water and soap, as well as areas where human waste mixes with soil, contribute to the spread of ascariasis. Occupation: Those who work with soil, such as farmers, are at higher risk. Travel: Visiting areas with poor sanitation and hygiene increases the chances of contracting ascariasis. Ascariasis causes severe complications in children, including malnutrition, intestinal blockages, and slowed growth. Maintaining good hygiene habits is most crucial. What are the Complications of Ascariasis? While in most cases of ascariasis are mild and don't cause major problems, heavy infestations can lead to severe complications, including: Intestinal blockage: A heavy ascariasis infestation might lead to a mass of worms blocking your intestines, causing severe cramping and vomiting. In extreme cases, the blockage can cause a hole in the intestinal wall or appendix, leading to internal bleeding or appendicitis. Duct blockages: The worms may obstruct the narrow ducts of your liver or pancreas, causing intense pain. Nutritional deficiencies: Infections can result in loss of appetite and poor absorption of nutrients, particularly affecting children's growth as they might not receive sufficient nutrition. How is Ascariasis Diagnosed? Doctors usually diagnose ascariasis by examining a stool sample for parasites and eggs. If you exhibit symptoms like abdominal pain or vomiting worms, your doctor might request an imaging test such as an X-ray, CT scan, ultrasound, MRI scan, or endoscopy to assess the severity of the infestation. How is Ascariasis Treated? Ascarisis treatment includes a course of antiparasitic drugs to eliminate the worms from the body. In severe cases, where a heavy infection results in a complete blockage in the intestines, a surgical intervention may be required to remove the blockage and prevent further complications, ensuring proper digestive health. Can I Prevent Ascariasis? Preventing ascariasis primarily involves practising good hygiene. Here are some tips: Always wash your hands with soap and water before eating or handling food Boil or filter water in regions that lack sanitation infrastructure Avoid consuming raw fruits and vegetables unless you can wash and peel them yourself Instruct children on the importance of washing hands frequently What is the Long-Term Outlook for an Ascariasis Infection? Many people recover from ascariasis with minimal treatment, symptoms may disappear before you're completely rid of the worms. However, larger infestations can cause serious complications. Therefore, if you suspect you have contracted ascariasis, it's important to consult a healthcare provider immediately. What Happens If Ascariasis is Left Untreated? If left untreated, the ascariasis worms can live inside your body for a year or two, which might lead to severe complications like intestinal blockage and nutritional deficiencies. Hence, early diagnosis and treatment are essential. Conclusion Navigating through the world of parasitic infections like ascariasis might seem daunting. Still, with the right knowledge and medical interventions, managing this conditions is entirely possible. Metropolis Healthcare is a leading diagnostic chain across India, known for its accurate pathology testing services. Our team of qualified blood collection technicians visit your home to collect samples. Test reports are easily shared online through email and our user-friendly Metropolis TruHealth app. We are dedicated to empowering patients to prioritise their health with reliable results and personalised care.
Subdural Hematoma: Causes, Symptoms, and Treatment
What is Subdural Hematoma? Imagine this scenario: you were playing football with friends and had a hard fall. A few weeks later, you start experiencing severe headaches and confusion. Could there be a connection? There might be more happening under your skull than you realise. In simple terms, a subdural hematoma is bleeding inside the head. It occurs when blood gathers in the space beneath the dura mater, one of the three layers which protects your brain and spinal cord. Think of these layers as protective cushions around your brain: the outer layer is the dura mater (closest to the skull), the middle layer is the arachnoid mater, and the innermost layer is the pia mater (closest to the brain tissue). When a blood vessel breaks in this area due to reasons like a head injury, the leaking blood causes a subdural hematoma. Notably, it falls under the category of traumatic brain injury (TBI) and can even prove fatal without immediate medical intervention. Let's now look at the different types of subdural hematomas that exist. What are the Types of Subdural Hematomas? The classification of subdural hematomas depends on three main factors: how quickly they develop, the extent of bleeding, and the damage they inflict. Consequently, we have three types: Acute Subdural Hematomas: This is the most dangerous type, in which severe symptoms appear immediately after a head injury, often within minutes to hours. Without quick diagnosis and treatment, it could cause unconsciousness, paralysis or even death. Subacute Subdural Hematomas: Develops within two to 10 days of a head injury. Symptoms usually emerge hours to weeks after the head injury. These hematomas often accompany concussions. Chronic Subdural Hematomas: Common in people over 65 years old, these result from slow bleeding and delayed symptom development. Even minor head injuries can cause chronic subdural hematomas. How common are Subdural Hematomas? Subdural hematomas aren't rare - they occur in approximately 1 in 4 people with head injuries. Therefore, it's important to understand their subdural hematoma symptoms to seek immediate medical help when needed. What are the Symptoms of Subdural Hematoma? Subdural hematoma symptoms can vary greatly based on the size of the hematoma, how quickly the bleeding occurs, and the person's overall health. Common symptoms include: Headache: Often the most prominent symptom, which may be persistent and worsen over time Nausea and Vomiting: Patients may experience gastrointestinal distress due to increased intracranial pressure Drowsiness: Individuals may feel unusually sleepy or have difficulty staying awake Confusion: Altered mental status can manifest as confusion, disorientation, or difficulty concentrating Dizziness or Balance Issues: Affected individuals may have trouble maintaining balance or feel lightheaded Slurred Speech: Communication difficulties may arise, impacting clarity and coherence Seizures: Some patients may experience seizures as a result of increased pressure on the brain Weakness or Numbness: Typically observed on one side of the body, which may indicate neurological impairment Vision Problems: This can include blurred or double vision, impacting the ability to see clearly Loss of Consciousness: In severe cases, individuals may become unresponsive or enter a coma It's crucial to seek medical attention if these symptoms arise, especially following a head injury. What Causes Subdural Hematomas? A subdural hematoma primarily results from a head injury due to a fall, vehicle collision, or assault. Think of it this way: the sudden blow to the head tears blood vessels that run along the brain's surface, leading to an acute subdural hematoma. People playing contact sports like football or boxing are particularly at risk, as are newborn infants due to their soft skulls. Moreover, individuals with bleeding disorders or those on blood thinners also face a higher risk of developing a subdural hematoma. What are the Risk Factors for Subdural Hematoma? Aside from the subdural hematoma causes mentioned above, certain risk factors elevate the chances of a subdural hematoma. These include: Age over 60 years Chronic alcoholism Long-term use of anticoagulants History of falls or repeated head injuries How is Subdural Hematoma Diagnosed? A CT scan is commonly used to diagnose a subdural hematoma. This scan combines X-rays and computer technology to produce detailed images of the inside of your body, helping to determine if there is any blood accumulation between your skull and brain. In certain situations, an MRI scan may be used as an alternative. How are Subdural Hematomas Treated? Subdural hematoma treatment primarily depends on the size, location, and severity of the hematoma, as well as the patient's overall health. The primary goal of treatment is to relieve pressure on the brain and prevent further complications. The most common procedure is craniotomy, in which a particular section of the skull is removed to access the hematoma directly. The surgeon will drain the blood, and the skull is replaced afterward. For smaller or asymptomatic hematomas, doctors may opt for observation and regular monitoring, allowing the body to reabsorb the blood naturally over time. In cases of large or symptomatic hematomas, surgical intervention is often required. Possible Surgery Complications Surgery carries inherent risks. Possible subdural hematoma complications can include infection, excessive bleeding, or brain swelling. Additionally, patients may also experience neurological deficits post-surgery, such as weakness or changes in speech, depending on the hematoma's location and the brain areas affected. In some cases, repeat surgery may be necessary if the hematoma re-accumulates. Patients should also be aware that they may experience cognitive or physical impairments during recovery, which might necessitate rehabilitation therapies to regain lost functions. Recovering from a Subdural Hematoma Recovery from a subdural hematoma varies significantly based on individual factors, including age, overall health, and the extent of the hematoma. After surgery, patients typically undergo a rehabilitation program tailored to their needs. This may involves a physical therapy, occupational therapy, and speech therapy to address any deficits. Ongoing medical follow-up is essential to monitor recovery and manage any long-term effects. Some individuals may experience fatigue, headaches, or mood changes during the recovery phase, which can last weeks to months. Support from family and caregivers plays a vital role in the healing process, ensuring a smoother transition back to daily life. What is Outlook for Someone with a Subdural Hematoma? The recovery time varies from individual to individual – while some people might recover in a few weeks, others may not fully recover at all. What are the Complications of Subdural Hematoma? Subdural hematoma complications can differ in severity and impact the patient's recovery. One of the most common issues is increased intracranial pressure, leading to headaches, nausea, and potentially loss of consciousness. Other complications includes seizures, neurological deficits, as well as cognitive impairments, which may result from pressure on the brain or damage to brain tissue. In some cases, re-accumulation of blood may necessitate an additional surgical intervention. Additionally, patients may face long-term effects like memory issue, personality changes, and difficulty with coordination. Early diagnosis and treatment are important to reduce these complications and improving outcomes. Conclusion While subdural hematomas may seem serious, they can be managed effectively with timely medical intervention. Always consult your healthcare provider for personalised advice and treatment. For those who need regular health check-ups or looking for a reliable diagnostic services, Metropolis Healthcare's provides dependable pathology testing and the convenience of at-home sample collection, delivered right to your door. Take charge of your health today with Metropolis Healthcare—because every test is important for your well-being! For individuals who need regular health check-ups or diagnostic services, Metropolis Healthcare's offers reliable pathology testing and convenient at-home sample collection right at your doorstep. Take control of your health today with Metropolis Healthcare- because when it comes to health, every test matters!
Uremia: Symptoms, Causes, and Effective Treatment Strategies
What is Uremia? Uremia is a serious condition that occurs when the kidneys are unable to filter waste from the blood effectively, resulting in accumulation harmful of toxins in the bloodstream. This condition is commonly seen in people with advanced kidney disease or kidney failure. Uremia causes symptoms like fatigue, nausea, muscle cramps, confusion, and swelling, along with complications such as high blood pressure and heart issues. In healthy kidneys, waste products are filtered out and excreted through urine. However, when kidney function declines, these toxins build up and impact different bodily systems. Uremia is a medical emergency that often necessitates urgent treatment, such as dialysis or a kidney transplant, to remove harmful substances from the bloodstream. Early detection and treatment of kidney issues can help prevent uremia from developing. Managing underlying conditions like diabetes and a high blood pressure is also crucial in preventing kidney damage that could lead to uremia. At which stage of chronic kidney disease does Uremia occur? According to medical experts, uremia commonly occurs in the advanced stages (stage IV or V) of chronic kidney disease (CKD), at which point the kidneys have lost much of their function and cannot efficiently filter out waste materials from the body. How common is Uremia? While there are no precise statistics for uremia, but it’s less common in in individuals who receive regular care from a nephrologist. Healthcare providers usually intervene before or shortly after mild uremia symptoms appear, using treatments such as dialysis or kidney transplants. What are the symptoms of Uremia? Uremia symptoms can vary depending on the severity of the condition. Some common ones include: Fatigue and Weakness: The body feels drained due to accumulation of toxins in the blood. Loss of Appetite: Many patients experience a decrease in their desire to eat. Nausea and Vomiting: The buildup of waste can cause digestive issues. Metallic Taste in the Mouth: A common symptom linked to the presence of toxins is a metallic taste. Muscle Cramps: Often caused by electrolyte imbalances Itchy Skin: Uremia can lead to skin irritation and itching, a result of excess waste in the bloodstream. Swelling: Fluid retention in the hands, feet, or face is typical due to poor kidney function. Shortness of Breath: Fluid may build up in the lungs, making it difficult to breathe Confusion and Difficulty Concentrating: Uremia affects brain function, leading to cognitive issues. High Blood Pressure: Increased blood pressure due to fluid overload. Chest Pain: Can occur if the heart is affected by fluid buildup or high blood pressure. In severe cases, untreated uremia symptoms can cause more serious complications such as seizures and coma. What is the main cause of Uremia? The primary uremia cause is kidney failure, often resulting from chronic kidney disease. Conditions like diabetes and hypertension are identified as the most common causes of CKD which can eventually lead to uremia if left unchecked. Who is most likely to get Uremia? Individuals with chronic kidney disease (CKD) or kidney failure are most likely to develop uremia. Common uremia causes include diabetes, high blood pressure, and long-term use of medications that can damage the kidneys. People with autoimmune diseases like lupus, as well as individuals with a family history of kidney issues, are also at higher risk. Elderly adults are more vulnerable due to age-related declines in kidney function. If left untreated, they can lead to toxin buildup, causing uremia symptoms such as fatigue, nausea, and confusion, which indicate the need for urgent treatment. What are the complications of Uremia? If left untreated, uremia can cause severe complications such as anemia, excessive bleeding, skeletal problems, heart complications, decreased brain function (uremic encephalopathy), infertility, and malnutrition. How is Uremia diagnosed? Uremia diagnosis typically begins with a comprehensive medical history and physical examination, focusing on symptoms like fatigue, nausea, muscle cramps, and confusion. The doctor will order several tests to confirm the diagnosis and assess kidney function. One of the key tests is a blood urea nitrogen (BUN) test, which monitors the level of waste products in the blood. High levels of creatinine in the blood are indicative of poor kidney function and possible uremia. A glomerular filtration rate (GFR) test is used to evaluate how well the kidneys are filtering blood. A low GFR indicates reduced kidney function, which can lead to uremia. Urine tests may also be performed to check for abnormal levels of protein or waste, further supporting the uremia diagnosis. In some cases, imaging tests like an ultrasound or CT scan may be used to visualise the kidneys and detect any structural issues. These tests help determine the extent of kidney damage and guide treatment. Getting a prompt uremia diagnosis is important to avoid more complications. Once diagnosed, treatment usually involves dialysis or a kidney transplant to remove toxins from the blood and help the kidneys work properly again. What tests will be done to diagnose Uremia? Doctors use various tests for uremia diagnosis, including blood urea nitrogen (BUN) and creatinine tests to evaluate for waste levels in the blood. A glomerular filtration rate (GFR) test evaluates kidney function, while urine tests and imaging studies (like an ultrasound or CT scan) help identify any kidney damage or issues. Can Uremia be cured? Uremia cannot be fully cured, but it can be effectively managed with proper treatment. The underlying cause, whether kidney failure or severe kidney disease, requires ongoing care. Treatments such as dialysis help eliminate waste from the blood, which helps control uremia symptoms. In some cases, a kidney transplant can serve as a long-term solution by restoring normal kidney function. Although these treatments do not cure the condition, they can greatly improve patient’s quality of life. Early identification and management of underlying issues like diabetes or high blood pressure are key to preventing the progression of uremia. Are there any specific medications to treat Uremia? While medications do not directly treat uremia symptoms, they play a significant role in preventing other effects of uremia on the body. This may include replacement EPO for preventing anemia and providing supplements such as iron, calcium, and vitamin D. How can Uremia be prevented? Preventing uremia is primarily involves managing chronic kidney disease (CKD). This includes regular dialysis, managing blood pressure and diabetes, avoiding kidney-damaging drugs, following a heart-healthy diet, and maintaining a healthy weight. What is the outlook for people with Uremia? The outlook for those with uremia depends according to the underlying cause and how quickly treatment is initiated. With proper management, including options like dialysis or a kidney transplant, many individuals can enjoy a good quality of life. However, uremia is a serious condition that can result in life-threatening complications if not treated. Early diagnosis and management of the underlying issues such as diabetes or high blood pressure are essential for slowing kidney damage and enhancing long-term outcomes for individuals with uremia. How long can a person live with Uremia? Without dialysis or a kidney transplant, survival rates of individuals with severe uremia can be as low as a few days or weeks. However, with proper medical intervention and palliative care, these numbers can increase significantly. Should I make any changes to my diet for Uremia? A diet that is heart-healthy and low in sodium is typically recommended for individuals with chronic kidney disease (CKD). If the condition advances to an elevated potassium, phosphorus, or parathyroid hormone (PTH) levels, you may need to limit your intake of potassium, phosphate, and protein. In such cases, consulting a renal dietitian can be very beneficial. When to see a Doctor? It’s important to schedule regular appointments to monitor your kidney health if you have risk factors for kidney disease, including a history of kidney injury, high blood pressure, or changes in urination habits. Do not hesitate from seeking an immediate medical attention if you experience abnormal behavior, chest pain, difficulty concentrating or breathing, confusion, drowsiness, fatigue, nausea, or vomiting. Conclusion Uremia is a serious medical condition that requires immediate attention and appropriate care. Although it may appear overwhelming, gaining a clear understanding of the uremia symptoms, causes, and treatment options can significantly help in effectively managing the condition. In light of the information provided, consider consulting with Metropolis Healthcare for their at-home sample collection services. Their advanced diagnostic labs and skilled blood collection technicians ensure reliable pathology testing right at your doorstep. Remember to prioritise your health, as gaining knowledge and seeking timely intervention are crucial steps toward a healthier life.
Priapism: Causes, Symptoms, and Urgent Treatment Options
What is Priapism? Priapism is a rare but serious condition which is characterised by a prolonged erection of the penis, often occurring without any sexual stimulation. This full or partial erection can last for hours and may lead to distress, embarrassment, and serious health complications if not treated quickly. Priapism isn't merely an extension of sexual desire. It's a medical condition that warrants immediate attention, especially if an erection persists for more than four hours. The term "priapism" is derived from Priapus, a Greek god renowned for his oversized, permanent erection. However, the reality of priapism is far from divine; it's a medical emergency that could result in permanent damage if not treated promptly. What are the types of Priapism? There are two main types of priapism: ischemic and nonischemic priapism. Ischemic Priapism, also known as low-flow priapism, occurs when blood becomes trapped in the penis due to inadequate venous drainage or malfunction of smooth muscles within the erectile tissue. Ischemic priapism is more common and requires immediate medical attention to prevent tissue damage due to lack of oxygen. Nonischemic Priapism, also known as high-flow priapism, occurs when there is an unregulated blood flow into the penile tissues due to injury or trauma. In this type, the penile tissues continue to receive some oxygen supply. A less common form is stuttering priapism, characterised by recurrent episodes of prolonged erections that are more frequently seen in men with sickle cell disease. How Common is Priapism? Although priapism is quite rare, it is more common in certain groups, particularly those with sickle cell disease, affecting about 30% to 45% of these individuals. It usually affects males aged 30 and older, but can also emerge during childhood among males with sickle cell disease. Despite its rarity, the seriousness and potential health implications demand that everyone stay informed about this condition. What are the Symptoms of Priapism? Priapism symptoms vary based on its type. In ischemic priapism, symptoms include an erection lasting more than four hours that is not related to sexual arousal, a rigid shaft of the penis (while the tip remains soft), and increasing pain in the penis. Nonischemic priapism features an erection lasting over four hours without sexual stimulation, but the penis isn't completely rigid. This condition is usually less painful than ischemic priapism. What is the Main Cause of Priapism? The root priapism cause remains unknown in 33% of all cases. However, several health conditions and factors could trigger this condition. It includes conditions like sickle cell disease, blood cancers such as leukemia, malaria, thalassemias, and penile cancer, along with spider bites and carbon monoxide poisoning. In addition, certain medications for erectile dysfunction and certain recreational drugs can also lead to priapism. Is Priapism Contagious? Priapism isn’t contagious. It doesn't spread through sexual intercourse or any form of contact with a person experiencing it. It's a strictly physiological condition arising from specific underlying health issues or triggers. Who Does Priapism Affect? Priapism can affect in anyone with a penis across all age groups, (even very rarely in newborns). It's seen most commonly in two specific age groups: children aged 5 to 10 and adults between 20 and 50 years old. What are the Complications of Priapism? If not treated, priapism causes can permanent damage to the penis. The trapped blood will eventually run out of oxygen, harming the penile tissues. Ongoing priapism can lead to tissue damage and may result in erectile dysfunction. Therefore, it's important to seek emergency care if an erection lasts longer than four hours. How is Priapism Diagnosed? Diagnosing priapism starts with a thorough review of medical history and a physical examination. The healthcare provider may ask about how long the erection has lasted, any previous medical conditions or injuries related to the genital area, and the use of medications or recreational drugs. Additional diagnostic tests recommended includes blood tests, urinalysis, and Doppler ultrasounds, to identify what triggered priapism symptoms. What Tests will be Done to Diagnose Priapism? To diagnose priapism definitively, healthcare providers may take a small blood sample from the penis to measure its oxygen level. The colour of this blood can help determine whether it is ischemic or nonischemic priapism. A Doppler ultrasound can also be used to evaluate blood flow in the vessels. In certain cases, a toxicology screen might be conducted to detect any substances that could be contributing to the priapism. How Do You Fix Priapism? Priapism is a medical condition characterised by an extended and painful erections that can persist for hours without sexual arousal. It is important to understand these priapism symptoms, such as an erection lasting longer than four hours, to ensure timely treatment. If left untreated, priapism can result in permanent damage to the erectile tissue and may cause erectile dysfunction. The approach to priapism treatment differs based on its type: ischemic priapism, which involves low blood flow, or non-ischemic priapism, which involves high blood flow. For ischemic priapism, where blood becomes trapped in the penis, immediate intervention is essential. Healthcare providers may apply a cold compress to reduce swelling and numb the area. They often perform a penile aspiration, a procedure that involves using a needle and syringe to draw out excess blood from the penis. In some cases, medication such as phenylephrine may be injected to constrict blood vessels and alleviate the erection. Non-ischemic priapism, usually resulting from trauma or injury, may resolve on its own but can be treated with observation or surgery if needed. Understanding the priapism causes, like certain medications, blood disorders, or nerve injuries, can aid in prevention and timely management, leading to better outcomes for those affected. Will Masturbating Make Priapism Go Away? In some cases, masturbation or sexual intercourse may provide temporary relief from the erection. However, these methods are not reliable priapism treatments and won’t solve the underlying problem. It is important to seek immediate medical help if you experience a persistent and painful erection. How Soon After Treatment Will I Feel Better? The recovery period from priapism largely depends on its cause and severity, and how promptly it was treated. In minor instances, relief could be immediate post-treatment. However, in severe priapism cases where surgical intervention was required, recovery might take longer. Can Priapism be Prevented? Prevention is indeed better than cure; but when it comes to priapism, it’s not always applicable. This is because a large proportion of cases occur without a known cause. Understanding the potential triggers can help manage the condition and reduce its frequency. Certain health conditions like sickle cell disease, blood cancer (leukemia), and malaria are known to result in low-flow priapism. Recreational drug use and certain medications can also trigger this condition. Therefore, managing these conditions and avoiding the misuse of such substances can indirectly help prevent priapism. It’s also important to understand that priapism is not contagious, so it cannot be spread through sexual intercourse. How Long Does Priapism Last? An erection lasting longer than four hours is considered as priapism. In some instances, there may be recurring episodes of prolonged erections, which are known as stuttering or intermittent priapism. Remember that any erection lasting more than four hours without any sexual stimulation should be considered a medical emergency. The trapped blood can reduce oxygen supply to the penile tissues, potentially causing serious complications if not treated quickly. What is the Outlook for Priapism? When managed effectively and promptly, the outlook for priapism can be quite positive. An early intervention help in preventing a permanent damage to the penis and safeguard sexual function. Delaying priapism treatment can result in erectile dysfunction and other complications. This emphasises the importance to seek a prompt medical attention if you think you are experiencing symptoms of priapism. How Do I Take Care of Myself if I Have Priapism? Living with priapism requires some lifestyle adjustments, awareness, and prompt medical treatment when necessary. Here are some practical tips: Be Observant: Monitor your body for any signs that could indicate priapism, like an erection lasting longer than normal or occurring without sexual arousal. Seek immediate medical attention: If symptoms occur, consult your healthcare provider immediately. Early treatment is essential to prevent complications related to priapism. Maintain a healthy lifestyle: Regular exercise, a balanced diet and adequate sleep contribute to overall health which can help manage associated conditions like sickle cell disease or blood cancer. When to See a Doctor? If you have an erection lasting more than four hours, seek emergency care. This duration is considered as the critical time frame after which damage to penile tissue could set in. Also, if you experience recurrent, persistent, painful erections that resolve on their own, consult your doctor as this may indicate stuttering priapism. Can I Get Priapism While I’m Sleeping? Yes, episodes of priapism can happen during sleep. However, it's important to remember that morning erections lasting no more than 30 minutes are normal and do not qualify as priapism. Conclusion Understanding priapism causes and symptoms of priapism is important for seeking a prompt medical attention. Being proactive about your health and making an informed choices can help prevent complications related to priapism. If you are looking for a dependable diagnostic services for blood tests associated with conditions leading to priapism like sickle cell disease or blood cancer, you can consider Metropolis Healthcare. Their team of qualified blood collection technicians can collect samples from your home, and their advanced laboratories provide accurate test results, which are conveniently shared online through email and the TruHealth app. Metropolis Healthcare is your trusted partner in prioritizing your health.
Osteomalacia: Symptoms, Causes, and Treatment Options
What is Osteomalacia? Osteomalacia, commonly referred as soft bones, is a medical condition characterised by the softening of bones. This often arises from a problem that causes vitamin D deficiency. Vitamin D plays a significant role in absorption of calcium, an essential mineral necessary for maintaining the strength and hardness of bones. In children, this condition is referred to as rickets. What are the Symptoms of Osteomalacia? Osteomalacia symptoms might not be noticeable initially, as they tend to emerge gradually. However, as the condition advances, individuals may begin to experience: Widespread bone pain, especially in the hips Muscle weakness that can interfere with daily activities Bone fractures that happen without major injury Additionally, individuals may also feel numbness around the mouth or tingling sensations in their arms and legs due to low calcium levels in the blood. Cramps or spasms occurring in the hands and feet may also be linked to this condition. What are the Causes of Osteomalacia? Osteomalacia is a condition characterised by the softening of bones due to inadequate mineralisation, primarily caused by deficiencies in essential nutrients. A primary osteomalacia causes is insufficient vitamin D, which is crucial for calcium absorption in the intestines. Without sufficient vitamin D, bones cannot mineralise properly, resulting in weakness, pain, and a higher risk of fractures. Alongside vitamin D deficiency, inadequate dietary intake of calcium and phosphate can significantly contribute to osteomalacia. These minerals are vital for preserving bone density and strength. Conditions impairing the nutrient absorption, such as celiac disease, inflammatory bowel disease, or those resulting from a gastric bypass surgery, can also lead to osteomalacia. Certain medications can worsen the problem; for an instance, some anticonvulsants can interfere with vitamin D metabolism, increasing the risk of osteomalacia. Additionally, genetic factors can play a role; rare inherited disorders may affect how the body processes vitamin D and essential minerals necessary for bone health. Chronic conditions like chronic kidney disease or liver disease can affect the balance of minerals in the body, contributing to the development of osteomalacia. Grasping the different osteomalacia causes is crucial for developing effective prevention and treatment strategies. This includes dietary changes, supplementation, and addressing underlying health conditions to restore bone health and avoid complications. What are the Treatments for Osteomalacia? Osteomalacia treatment primarily focuses on addressing the underlying causes of osteomalacia. Supplements of vitamin D, calcium, and phosphorus may be recommended for individuals who have difficulty absorbing nutrients through their intestines. People with certain conditions may require regular blood tests to monitor their phosphorus and calcium levels. Getting adequate exposure to sunlight could also help improve vitamin D levels naturally. With appropriate treatment, many individuals with vitamin D deficiency disorders might notice improvements within weeks. Generally, full recovery typically occurs within six months. What are the Potential Complications of Osteomalacia? If left untreated, osteomalacia can lead to serious complications that can greatly affect a person's quality of life. One of the most concerning complications is the heightened risk of bone fractures, especially in the ribs, spine, and legs. Weakened bones become more susceptible to breaking, even from slight injuries or falls. Another potential complication is the development of pseudofractures, also known as Looser's zones. These are partial cracks in the bones that can be very painful and make walking difficult. In severe cases, these cracks can progress to fractures. Muscle weakness and pain are typical symptoms of osteomalacia, which can result in difficulties with walking and a waddling gait. This can have a substantial effect on a person's mobility and independence. In some rare cases, untreated osteomalacia can result in bone deformities, especially in children whose bones are still developing. Without timely intervention, the symptoms of osteomalacia may worsen over time, increasing the risk of complications and adversely affecting quality of life. How is Osteomalacia Diagnosed? Diagnosing osteomalacia involves a comprehensive approach combining medical history, physical examination, and various diagnostic tests. Initially, a healthcare provider will gather information about the patient's symptoms, which might include bone pain, muscle weakness, and difficulty walking. Since these symptoms can be unclear and progress slowly, it may take years for a diagnosis. Blood tests play a crucial role in the diagnostic process, usually assessing levels of calcium, phosphate, and vitamin D. An elevated level of alkaline phosphatase (ALP) and parathyroid hormone (PTH) can also indicate the presence of osteomalacia. A 24-hour urine test can also be performed to assess the excretion of calcium and phosphate. Imaging studies, such as X-rays, can highlight distinctive signs of osteomalacia, including pseudofractures referred to as Looser's zones. In some cases, a bone biopsy may be conducted to examine the mineralisation of bone tissue directly. Overall, an accurate diagnosis often requires a combination of these methods to confirm osteomalacia and rule out other conditions affecting bone health. An early diagnosis is essential for effective treatment and recovery. What Should I Eat if I have Osteomalacia? Diet is crucial in managing osteomalacia. It’s essential to prioritise a nutrient-rich diet that support bone health, particularly emphasising calcium, vitamin D, and phosphate. These include: Milk and Yogurt: These are excellent sources of calcium and vitamin D. Opt for fortified varieties if available. Paneer (Cottage Cheese): A good source of calcium and protein Spinach, Broccoli, and Mustard Greens: These vegetables provide calcium and other essential vitamins. However, be cautious with spinach as it contains oxalates that can inhibit calcium absorption. Fatty Fish: Include options like sardines or mackerel, which are rich in vitamin D. Almonds and Walnuts: These provide both calcium and healthy fats. Rajma (Kidney Beans) and Chole (Chickpeas): High in protein and can help meet dietary needs Fortified Cereals: Choose cereals fortified with vitamin D and calcium. Oranges and Kiwi: These fruits can provide vitamin C, which is beneficial for bone health. Including these nutrient-rich foods in your diet can significantly improve bone health and help in managing osteomalacia. Prioritising calcium, vitamin D, and phosphate, along with medical advice, is crucial for overall well-being. FAQs Is Osteomalacia the same as Osteoporosis? Although both conditions involve weakened bones, they are not the same. Osteoporosis affects already formed, living bone, whereas osteomalacia impacts the hardening process of new bone formation. Are there different types of Osteomalacia? Yes, osteomalacia can differ depending on the specific nutritional deficiency that leads to it, such as a lack of vitamin D or phosphate. Is Osteomalacia the same as Rickets? Though both conditions result in weak and soft bones due to nutrient deficiencies, rickets specifically affects new bone growth in children. On the other hand, osteomalacia can develop in adults and children. Conclusion Understanding osteomalacia, its potential causes, identifying its symptoms, and knowing your treatment options are all crucial steps towards safeguarding your bone health. If you suspect you may have this condition, it's important to consult a healthcare professional. At Metropolis Healthcare, we offer advanced diagnostic services to facilitate the early detection of various health issues. Our skilled technicians offer at-home blood sample collection for your convenience. You can access your reports quickly online through email or the convenient Metropolis TruHealth app. Prioritize your well-being with reliable results and customized care from Metropolis Healthcare.
Trigeminal Neuralgia: Symptoms, Causes, Treatments and More
Living with pain can be an daunting experience. If the pain can be sudden, severe, and primarily affects the face, it could be a medical condition called Trigeminal Neuralgia. This condition can significantly disrupt daily life, as simple activities like chewing, talking, or even smiling can provoke intense pain. But don’t worry; this article intend to help you understand Trigeminal Neuralgia, covering its symptoms, causes, and possible treatment options. We will also discuss strategies to effectively manage your symptoms, enabling you to maintain a near-normal life despite this condition. What is Trigeminal Neuralgia? Trigeminal neuralgia (TN) is a neuropathic condition which is characterised by an intense facial pain that can severely disrupt daily activities. The root cause of this disorder lies in the trigeminal nerve, which is situated near the brainstem. This nerve plays a crucial role in transmitting sensation to your face and head. Pain associated with trigeminal neuralgia can be triggered by simple actions such as talking, chewing, or even brushing your teeth. Although it is not life-threatening, the condition can profoundly affect your quality of life, leading to significant challenges in your lifestyle and emotional well-being. Pursuing an appropriate treatment can help manage symptoms effectively. How common is Trigeminal Neuralgia? Trigeminal neuralgia affects approximately 0.03% to 0.3% of the global population, with women being three times more likely to experience it than men. While it typically begins in people over 50, it can occur at any age, affecting individuals of any age, from various backgrounds and lifestyles. What are the Symptoms of Trigeminal Neuralgia? The main symptom of trigeminal neuralgia is intense facial pain, often described as an electric shock or stabbing sensation. This pain typically affects one side of the face and may be accompanied by muscle spasms during attacks. Between these painful attacks, patients might experience various sensations, including: Burning sensations: A persistent feeling of burning in the face, often uncomfortable. Throbbing: Intermittent, pulsing pain that can disrupt concentration. Numbness: A feeling of loss of sensation in the facial area, which may accompany pain. Dull aches: Continuous, less intense pain that can be draining and affect daily activities. There are two types of trigeminal neuralgia, distinguished by their symptoms: Classic Trigeminal Neuralgia: Characterised by sudden, severe bursts of shooting facial pain. Atypical Trigeminal Neuralgia: Involves a constant burning sensation paired with sharp pain. Trigeminal Neuralgia Symptom Triggers Symptoms can be triggered by simple facial movements or everyday activities, making the condition particularly challenging to manage. Common triggers include: Washing your face or applying makeup: These routine tasks can cause sudden pain, making personal care difficult. Eating or Drinking: The act of chewing or swallowing can provoke painful sensations, leading some individuals to avoid meals. Brushing your teeth or Flossing: Oral hygiene routines can become daunting when they trigger sharp pain in the face. Talking or Smiling: Even expressions of happiness or communication can lead to uncomfortable pain episodes, causing individuals to withdraw socially. Encountering a Breeze or Gust of Wind on your face: Environmental factors, such as wind, can unexpectedly trigger painful episodes, limiting outdoor activities. Interestingly, people rarely experience painful attacks while they are sleeping, which can provide some relief. Understanding more about these symptoms and what triggers them can help individuals manage their condition better. By avoiding activities that cause pain, they can improve their overall comfort and quality of life. What Causes Trigeminal Neuralgia? Trigeminal neuralgia typically arises from pressure on or damage to the trigeminal nerve, which is responsible for facial sensation. Healthcare providers classify this condition into two main types based on the underlying cause. Primary or Classic Trigeminal Neuralgia occurs when a blood vessel exerts pressure on the trigeminal nerve near the brainstem. This pressure disrupts the nerve's normal function, leading to episodes of severe facial pain. On the other hand, secondary trigeminal neuralgia is caused by an underlying condition that impacts the trigeminal nerve. It may involve diseases like multiple sclerosis, which harms the nerve's protective covering, or a tumor that physically affects the nerve. Recognising these classifications helps in diagnosing the condition and identifying the most suitable treatment options for those suffering from trigeminal neuralgia. What are the Risk Factors for Trigeminal Neuralgia? Certain factors may increase your chances of developing trigeminal neuralgia, including: High blood pressure Smoking Aging Female Sex Family History of TN How is Trigeminal Neuralgia Diagnosed? Diagnosing trigeminal neuralgia requires an in-depth discussion about your symptoms and medical history, along with a thorough physical examination. During this process, healthcare providers focus on several key factors to determine the diagnosis: The specific type of pain you are experiencing, such as sharp or stabbing sensations. The exact location on your face where the pain occurs, which can provide important clues. The activities or movements that trigger a painful episode, aids to identify potential triggers. To rule out other causes of facial pain, like migraines or cluster headaches, doctors might recommend a brain MRI. This scan helps confirm the diagnosis and enables doctors to select the best treatment options for your condition. What is the Treatment for Trigeminal Neuralgia? Treatment for trigeminal neuralgia can include a combination of medications, surgery, and other therapies. Medication for Trigeminal Neuralgia Pharmacotherapy is frequently the first line of treatment for trigeminal neuralgia (TN), focusing on relieving pain and improving the patient's quality of life. This approach may include several types of medications: Antiseizure Medications: Often prescribed because they can effectively block pain signals in the nervous system. However, it’s important to know that its effectiveness may decrease over time, which might require changing the dosage or switching to different treatments. muscle relaxant: Option used to alleviate the symptoms of trigeminal neuralgia. It works by reducing muscle spasms and can provide additional pain relief for some patients. While these medications can be effective, they also lead to some potential side effects, including dizziness, fatigue, or gastrointestinal issues. Your healthcare provider will work closely with you to evaluate your symptoms and medical history, helping you choose the most suitable medication based on your individual case and needs. Regular follow-ups are essential to monitor the treatment's effectiveness and make necessary adjustments. Surgery for Trigeminal Neuralgia If medications don't help relieve pain, surgery for trigeminal neuralgia could be a viable option. This procedure requires a lot of precision because the area it targets is small. So, it's important to find experienced neurosurgeons who specialize in this type of surgery to ensure the best results. Other treatments for trigeminal neuralgia Your healthcare provider may recommend other treatments to help manage trigeminal neuralgia pain, usually alongside medication. These options can include botulinum toxin injections or nerve blocks for temporary relief, as well as acupuncture, biofeedback, talk therapy, yoga, meditation, and aromatherapy. Using these treatments can improve pain relief and enhance your quality of life. What Can I Expect if I Have Trigeminal Neuralgia? Managing the condition of trigeminal neuralgia can be challenging due to its chronic nature and unpredictable pain attacks. However, with right treatment options, such as medication or surgery, you can still lead a comfortable life. While TN mainly affects the physical health, it can also take a toll on mental and emotional well-being. The fear of experiencing the painful episodes can lead some people to avoid activities or social situations. However, it’s important to remember that while managing this condition may be a long-term challenge, there are effective treatments available that can help you live a fulfilling and enjoyable life. What Are the Possible Complications of Trigeminal Neuralgia? If left untreated, trigeminal neuralgia can result in severe pain that significantly impacts daily life and overall well-being. This chronic discomfort can lead to mental health issues, such as depression and anxiety, as individuals may struggle to cope with the constant fear of pain attacks. The emotional impact can be just as difficult as the physical symptoms, emphasizing the need for prompt treatment to address both the pain and its psychological effects. This approach is crucial for improving overall quality of life and ensuring a more manageable and fulfilling existence. When To See A Doctor? If you experience sudden episodes of severe facial pain, it is essential to seek medical assistance without delay. Prompt diagnosis and treatment are vital, as they can help effectively manage symptoms and significantly enhance your overall quality of life and well-being. Conclusion Understanding trigeminal neuralgia offers an empowering step towards managing this condition effectively. With knowledge of its symptoms, causes, and available treatments, you are better equipped to take proactive steps regarding your health, leading to more informed decisions and improved quality of life. At Metropolis Healthcare, we are committed to supporting you on your health journey through our comprehensive diagnostic and blood testing services. Our team of qualified professionals provide at-home sample collection, ensuring your convenience and report accuracy. With our commitment on delivering reliable results and personalised care, you can prioritise your health with confidence. Remember, while trigeminal neuralgia can be an overwhelming condition, you are not alone. Consult with your healthcare provider for personalised advice and reach out to support groups for shared experiences and coping strategies. Always remember that prioritising your health is within reach with the right knowledge and medical care, and Metropolis Healthcare is here to assist you every step of the way.
 Home Visit
Home Visit Upload
Upload




















 WhatsApp
WhatsApp