Latest Blogs
Uterine Polyps: Causes, Symptoms, and Diagnosis
What are uterine polyps? Uterine polyps, also known as endometrial polyps, are soft growths that develop in the endometrium, the inner lining of the uterus. These polyps are usually benign (noncancerous) and can range in size from a few millimetres to several centimetres. They are typically attached to the uterine wall by a thin stalk or a broad base. Uterine polyps are made up of endometrial tissue, which includes glands, blood vessels, and connective tissue. In some cases, uterine polyps can contain smooth muscle cells as well. While most polyps are benign, a small percentage (less than 5%) may be precancerous or develop into cancer. Who is affected by uterine polyps? Uterine polyps can affect women of all ages but are most common in those going through or after menopause, with the highest occurrence between ages 40 and 50. Younger women can also develop polyps, especially if they have risk factors such as obesity, high blood pressure, or tamoxifen therapy for breast cancer. Hormone replacement therapy (HRT) and a family history of genetic disorders like Lynch syndrome may also increase the risk. While often benign, uterine polyps causes could include irregular bleeding or fertility issues. Early detection and medical evaluation are essential for appropriate treatment and management. Are uterine polyps common? Uterine polyps are a relatively common gynaecological condition. According to research, they occur in approximately 10% of women. The likelihood of developing uterine polyps increases with age, peaking in the fifth decade of life. After menopause, the incidence gradually declines. Uterine polyps causes are rarely seen in women under 20 years old. What are the symptoms of uterine polyps? While some women with uterine polyps may not experience symptoms, others can develop noticeable signs. The most common uterine polyps symptom is abnormal uterine bleeding, which may include heavy or irregular periods, spotting between cycles, or prolonged menstruation. Postmenopausal bleeding is another key concern, as any vaginal bleeding after menopause should be promptly evaluated to rule out polyps or more serious conditions like endometrial cancer. In some cases, uterine polyps can contribute to infertility by interfering with embryo implantation. Additionally, some women may experience unusual vaginal discharge, which can be watery or blood-tinged. These symptoms can vary in severity, and while uterine polyps are often benign, they can impact quality of life and reproductive health. If you notice persistent abnormal bleeding, unexpected vaginal discharge, or fertility concerns, it’s essential to consult a healthcare provider. Early uterine polyps diagnosis through ultrasound, hysteroscopy, or biopsy can help determine the appropriate uterine polyps treatment and ensure better health outcomes. Are uterine polyps painful? In most cases, uterine polyps do not cause significant pain. However, some women with larger polyps may experience mild discomfort or a feeling of heaviness in the lower abdomen or pelvis. Rarely, uterine polyps can twist or become infected, leading to acute pain. If you have severe or persistent pelvic pain, seek prompt medical attention. What causes uterine polyps? Exact uterine polyps causes are not fully understood, but several factors may contribute. Hormonal imbalances, particularly high oestrogen levels from obesity or hormone therapy, are a key factor. Genetic mutations, such as those linked to Lynch syndrome, can also increase risk. Additionally, chronic inflammation of the endometrium is another potential uterine polyps cause. How are uterine polyps diagnosed? Uterine polyps diagnosis involves a combination of imaging tests and tissue sampling to confirm their presence and rule out other conditions. If a healthcare provider suspects the condition based on uterine polyps symptoms such as abnormal bleeding or infertility, they may recommend several diagnostic procedures. A transvaginal ultrasound is often the first step, using sound waves to create images of the uterus and detect polyps. For a more detailed view, a hysteroscopy may be performed, where a thin, lighted tube is inserted through the cervix to directly examine the uterine lining. An endometrial biopsy may also be conducted, where a small tissue sample is taken from the uterus for laboratory analysis to determine whether the polyp is benign or cancerous. Another option is saline infusion sonohysterography (SIS), which involves injecting sterile saline into the uterus before an ultrasound to enhance visibility. Once a uterine polyps diagnosis is confirmed, appropriate uterine polyps treatment, such as medication or surgical removal, can be recommended based on the patient’s condition and symptoms. The choice of diagnostic method depends on the individual's medical history, symptoms, and overall health to ensure accurate detection and effective management. How are uterine polyps treated? Uterine polyps treatment varies based on factors like age, symptoms, and the size and location of the polyps. If polyps are small, asymptomatic, and the patient is premenopausal, a doctor may suggest watchful waiting, where the polyps are monitored over time without immediate intervention. However, if uterine polyps symptoms such as abnormal bleeding or fertility issues occur, removal may be necessary. One common procedure is hysteroscopic polypectomy, a minimally invasive surgery where a hysteroscope is used to visualise and remove the polyps. This procedure is typically performed under general or local anaesthesia with sedation. Another option is dilation and curettage (D&C), where the uterine lining and polyps are scraped away. In cases of multiple or recurrent polyps, hormonal medications like progestins or gonadotropin-releasing hormone agonists (GnRHa) may be prescribed to shrink polyps and reduce the chance of regrowth. While medication can help manage symptoms, it is not always a permanent solution, and polyps may return once treatment stops. Following uterine polyps treatment, doctors may recommend follow-up visits or imaging tests to monitor for recurrence. Regular check-ups are especially important for postmenopausal women or those with risk factors for endometrial abnormalities to ensure long-term reproductive and overall health. Do uterine polyps need to be removed? The decision to remove uterine polyps depends on several factors, including: Symptoms: If you are experiencing abnormal bleeding, infertility, or other symptoms related to polyps, removal is usually recommended. Size and location: Large polyps or those that are causing obstruction may need to be removed. Age and menopausal status: Postmenopausal women with polyps are at a higher risk of precancerous or cancerous changes, so removal is often advised. Fertility concerns: Polyps can interfere with fertility, so removal may be recommended for women trying to conceive. Is uterine polyp removal painful? If your doctor recommends surgical removal of uterine polyps, a common concern is whether the procedure will hurt. Fortunately, uterine polyp treatment via polypectomy is usually performed under anaesthesia, greatly reducing discomfort. Some women report mild cramping or light bleeding afterwards, but significant post-procedure pain is rare. Can uterine polyps be prevented? Currently, there are no proven ways to completely prevent the development of uterine polyps. However, you can take steps to reduce certain risk factors by maintaining a healthy weight to minimise excess estrogen exposure. You should also engage in regular physical activity, eat a balanced diet rich in fruits, vegetables, and whole grains, and discuss hormone replacement therapy risks and benefits with your doctor. What can we expect if we have uterine polyps? If diagnosed with uterine polyps, you may experience irregular menstrual bleeding, postmenopausal bleeding, or infertility. However, some women have no symptoms, and polyps are often found during routine exams. They vary in size, with larger polyps more likely to cause bleeding. Uterine polyps treatment typically involves surgical removal, especially if they cause symptoms or appear abnormal. Your doctor will tailor a treatment plan based on your age, symptoms, and reproductive goals. Should we worry about uterine polyps? While finding out you have uterine polyps can feel alarming, it's important to know that around 95% of polyps are noncancerous. However, in rare cases, polyps can contain precancerous or cancerous cells. This is more likely after menopause. Any vaginal bleeding after menopause should be promptly evaluated. What percentage of uterine polyps are cancerous? Although any abnormal growth can feel worrisome, the vast majority of uterine polyps - more than 95% - are benign. Actual cancer is found in only about 1-5% of polyps. However, the risk is higher for postmenopausal women. Around 5-6% of uterine polyps in women after menopause contain precancerous or cancerous cells. Certain factors like obesity and high blood pressure can also increase the likelihood of malignancy. When to see a doctor? Be sure to consult your healthcare provider if you experience vaginal bleeding after menopause, irregular menstrual bleeding, such as heavy periods or spotting between cycles, bleeding after intercourse, or difficulty getting pregnant. These issues can stem from various gynaecological conditions, including uterine polyps. Conclusion Uterine polyps are a common gynaecological condition that can cause abnormal bleeding, infertility, and other symptoms. If you suspect you may have the condition, don't hesitate to consult with your healthcare provider. They can help you determine the best course of action, whether it's watchful waiting or uterine polyps removal surgery. At Metropolis Healthcare, we understand the importance of accurate diagnosis and personalised care. Our team of skilled phlebotomists can perform at-home sample collection for various tests, ensuring your comfort and convenience. With our state-of-the-art diagnostic laboratories and commitment to delivering reliable results, you can trust Metropolis Healthcare to support you on your journey to better reproductive health.
What is Toxic Shock Syndrome? Symptoms, Causes, and Risk Factors
What is toxic shock syndrome (TSS)? Toxic shock syndrome is a serious condition triggered by bacterial toxins. These toxins can cause a dramatic drop in blood pressure and lead to organ failure. TSS progresses rapidly and can be fatal if not treated promptly. While anyone can develop TSS, it gained attention in the 1970s-80s due to cases linked to high-absorbency tampons. Today, less than half of TSS cases are menstrual-related. While often associated with tampon use, TSS can impact men and children too. Knowing the signs and risk factors is crucial for early detection and prompt treatment. How common is toxic shock syndrome (TSS)? TSS is quite rare, affecting about 1 in 100,000 people in the United States. Historically more prevalent among menstruating women, nowadays less than half of TSS cases are linked to tampon use. Although rare, understanding TSS remains important for people of all ages and genders. What are the symptoms of toxic shock syndrome (TSS)? Toxic shock syndrome symptoms can manifest suddenly and worsen rapidly. Key signs include: High fever (above 102°F or 38.9°C) Low blood pressure Vomiting or diarrhoea Skin rash resembling a sunburn Confusion or disorientation Muscle aches Redness in the eyes, mouth, and throat Seizures Headaches If you experience any of these toxic shock syndrome symptoms, especially if you've recently used tampons or had surgery, seek immediate medical care. Early intervention is vital for successful toxic shock syndrome treatment. What causes toxic shock syndrome (TSS)? Toxic shock syndrome causes are mostly attributed to bacterial toxins produced by Staphylococcus aureus (staph) or Streptococcus pyogenes (strep) bacteria. While these bacteria often exist harmlessly on the skin or in the body, under certain conditions, they can multiply rapidly and release harmful toxins into the bloodstream, triggering a severe immune response. Toxic shock syndrome causes are commonly linked to the use of super-absorbent tampons, particularly when left in for prolonged periods, creating an environment that allows bacterial overgrowth. However, TSS is not limited to menstruation-related cases. It can also occur due to surgical wounds, cuts, burns, or childbirth, where bacteria enter the body and spread. Additionally, the use of contraceptive sponges or diaphragms may contribute to bacterial buildup, increasing the risk of infection. While certain factors heighten the likelihood of TSS, anyone, regardless of gender or age, can develop this life-threatening condition if exposed to the toxins. Early recognition of toxic shock syndrome symptoms such as fever, rash, low blood pressure, and organ dysfunction is critical for timely medical intervention and successful treatment. What bacteria cause toxic shock syndrome (TSS)? The primary bacteria responsible for TSS are: Staphylococcus aureus (staph): Commonly found on the skin and mucous membranes, staph bacteria are usually harmless but can cause TSS if they overgrow and produce toxins. Streptococcus pyogenes (strep): These bacteria cause strep throat and other infections. In rare cases, they can lead to a severe form of TSS called streptococcal toxic shock syndrome (STSS). Clostridium sordellii: This bacterium has been linked to a small number of TSS cases, primarily in postpartum women or individuals who recently had surgery. How long does it take to get toxic shock from a tampon? There's no set timeline for developing toxic shock syndrome from a tampon, but the risk increases the longer a tampon is left in. Most guidelines recommend changing tampons every 4-8 hours and using the lowest absorbency needed. Avoid using tampons overnight if possible. Doctors advise changing tampons frequently and alternating with pads to minimise TSS risk. If you notice a toxic shock syndrome rash, accompanied by fever or low BP, remove the tampon immediately and contact your doctor. How long does it take to have symptoms of toxic shock syndrome? Toxic shock syndrome symptoms can develop rapidly, usually within a few days after the bacteria enter the body. However, symptoms may take up to a week to appear. If you suspect TSS, don't wait for symptoms to worsen. Seek medical help right away, as prompt toxic shock syndrome treatment is crucial for the best outcome. Can sanitary pads cause toxic shock syndrome? While less common than with tampons, there have been reports of TSS linked to sanitary pad use. The key culprit is the bacteria, not the menstrual product itself. However, sanitary pads can create an environment conducive to bacterial growth if not changed regularly. To minimise risk, change pads every 4 to 8 hours and maintain proper hygiene. How is toxic shock syndrome (TSS) diagnosed? Diagnosing toxic shock syndrome requires a thorough evaluation, including a physical exam to check for fever, rash, and low blood pressure. Blood and urine tests help detect bacteria and assess organ function. If TSS is linked to tampon use, a pelvic exam may be performed. Doctors may also collect samples from the cervix, vagina, or throat to test for Staphylococcus aureus or Streptococcus pyogenes. A quick, accurate diagnosis is crucial for timely and effective toxic shock syndrome treatment. How is toxic shock syndrome (TSS) treated? Toxic shock syndrome treatment requires a comprehensive approach to eliminate the infection, stabilise the body, and prevent complications. Immediate medical intervention is crucial, as early treatment significantly improves recovery outcomes. Toxic shock syndrome treatment typically includes intravenous (IV) antibiotics to target the bacterial infection and IV fluids to counteract dehydration and low blood pressure. If a tampon, wound dressing, or contraceptive device is suspected as the infection source, it is promptly removed. Toxic shock syndrome medication may be administered to reduce fever and manage pain. In severe cases, hospitalisation in the intensive care unit (ICU) is necessary for close monitoring and advanced supportive care, including oxygen therapy or mechanical ventilation if organ function is compromised. Additional treatments, such as dialysis for kidney failure or surgery to remove infected tissue, may be required in extreme cases. With prompt medical attention, most individuals recover, but early recognition of symptoms is essential to prevent life-threatening complications associated with toxic shock syndrome. What are the complications of toxic shock syndrome if left untreated? Without prompt toxic shock syndrome treatment, TSS can rapidly progress and lead to severe, potentially fatal complications. Inadequate blood flow to vital organs can result in life-threatening shock. TSS can cause multiple organ dysfunction, including renal and liver failure. It can also cause sdult respiratory distress syndrome (ARDS), a serious lung condition that lead to breathing difficulties and low blood oxygen levels. Untreated toxic shock syndrome also has a high mortality rate. Can toxic shock syndrome (TSS) go away on its own? No, toxic shock syndrome does not resolve spontaneously and requires prompt medical intervention. The bacterial toxins responsible for TSS can cause rapid and severe damage to the body, making early treatment essential for preventing life-threatening complications. How can we prevent toxic shock syndrome (TSS)? While toxic shock syndrome can't always be fully prevented, certain precautions can reduce the risk. Use the lowest absorbency tampon needed, change tampons every 4-8 hours, and alternate with pads, especially at night. Proper wound care is crucial—keep cuts, burns, and scrapes clean and covered to prevent infection. Watch for signs of infection like redness or swelling. Lastly, be aware of TSS symptoms, such as fever, rash, and vomiting, and seek immediate medical attention if they occur. What are the risk factors for toxic shock syndrome (TSS)? Several factors can increase the risk of developing toxic shock syndrome. Using highly absorbent tampons or leaving them in for too long creates an environment where bacteria can thrive. Open wounds, burns, or surgical incisions provide pathways for bacteria to enter the body and cause infection. Viral illnesses like influenza or chickenpox may weaken the body’s defenses, increasing susceptibility to TSS. Additionally, individuals with weakened immune systems due to conditions like diabetes or chronic diseases are more vulnerable. Other risk factors include the use of contraceptive devices such as diaphragms or sponges, which can introduce bacteria into the body. While TSS is rare, recognising these risk factors can help reduce the likelihood of infection. Practicing proper hygiene, using tampons safely, caring for wounds properly, and staying aware of TSS symptoms can all contribute to prevention. What is the survival rate of toxic shock syndrome? Thanks to advancements in medical care, the survival rate for TSS has improved significantly in recent years. However, the exact prognosis can vary depending on factors such as the promptness of treatment, the patient's overall health, and the severity of the infection. When to see a doctor? Visit a doctor if you experience symptoms suggestive of toxic shock syndrome, such as high fever (38.9°C or higher), vomiting or diarrhoea, rash resembling a sunburn, muscle aches, or confusion or disorientation. Seek immediate medical attention, especially if you have recently used tampons or have a skin wound. Conclusion While toxic shock syndrome is rare, understanding its causes and symptoms is key to protecting your health. If you think you might have TSS, don't wait—get medical help immediately. Timely toxic shock syndrome treatment can make all the difference. At Metropolis Healthcare, we're committed to empowering you with the knowledge to make informed health choices. If you have concerns about toxic shock syndrome or any health issue, our expert team is here for you. With a nationwide network of diagnostic labs and convenient at-home sample collection, getting answers is simple. Book a health check-up or explore our comprehensive pathology services today.
Low Libido (Low Sex Drive)
What is low libido (low sex drive)? Low libido, or low sex drive, refers to a decreased interest in sexual activity that persists over time. It's characterised by a lack of desire for sex, reduced sexual thoughts or fantasies, and a general disinterest in initiating or engaging in sexual encounters. While it's normal for sexual desire to fluctuate throughout life, a prolonged period of low libido can cause concern and strain on relationships. It's important to note that libido meaning can vary from person to person. What one individual considers a "normal" level of sexual desire may differ from another's. However, if you find that your lack of interest in sex is causing distress or affecting your quality of life, it may be time to address the issue. While the prevalence may vary depending on age, health status, and other factors, it's clear that low libido is a widespread issue. How common is low libido? Low libido is a relatively common concern, affecting both men and women of all ages. According to a study published in the Journal of the American Medical Association, 43% of women and 31% of men reported experiencing sexual dysfunction, with low desire being a significant factor. What are the symptoms of low libido? The primary low libido symptom is a persistent lack of interest in sexual activity. Other signs may include rarely or never initiating sex, feeling reluctant to engage in sexual encounters, having few or no sexual thoughts or fantasies, difficulty becoming aroused or maintaining arousal, and feeling distressed or frustrated about your lack of sexual desire. If you're experiencing these low libido symptoms, it's essential to talk to a healthcare provider. What causes low libido? Low libido causes can be complex and multifaceted, involving a combination of physical, psychological, and relationship factors. Identifying the underlying reasons can help in finding effective solutions. Hormonal Imbalances In women, low libido or low sex drive is often linked to hormonal changes, particularly during menopause when oestrogen levels decline. This can lead to vaginal dryness, discomfort during sex, and a reduced desire for intimacy. Pregnancy, childbirth, and breastfeeding can also cause fluctuations in hormones that impact sexual interest. In men, low testosterone levels can contribute to decreased sex drive. While testosterone naturally declines with age, other factors such as obesity, chronic illness, and certain medications can also lower levels, leading to reduced libido. Psychological Factors Stress, anxiety, and depression are major contributors to low libido. Mental exhaustion, work pressure, or financial worries can make it difficult to focus on intimacy. Additionally, poor body image, low self-esteem, and a history of sexual trauma can negatively affect sexual desire. Relationship Issues Unresolved conflicts, lack of communication, and emotional disconnection can significantly impact libido. When partners feel distant or misunderstood, sexual desire may diminish. Furthermore, mismatched libidos between partners can create tension, further reducing interest in intimacy. Physical Health Conditions Chronic illnesses like diabetes, heart disease, and obesity can impact sexual function. Additionally, certain medications—especially antidepressants and blood pressure drugs—are known to have low libido as a potential side effect. Addressing these medical issues with a healthcare provider can help manage their impact on sexual health. Lifestyle Factors Low libido causes can also stem from unhealthy lifestyle habits. Excessive alcohol consumption, substance abuse, sleep deprivation, poor diet, and lack of exercise can lead to reduced energy levels and decreased sexual interest. Maintaining a healthy lifestyle by prioritising sleep, nutrition, and physical activity can help improve libido over time. Low libido in women For women, low libido can be particularly complex, influenced by a range of biological, psychological, and social factors. Hormonal fluctuations during menopause, pregnancy, or while using hormonal contraceptives can contribute to decreased desire. Additionally, pain during intercourse caused by conditions like vaginismus, endometriosis, or vaginal dryness may lead to avoidance of sexual activity. Psychological factors also play a role. Body image concerns, self-consciousness, and past negative experiences can make intimacy challenging. Stress from work, family responsibilities, or personal struggles may further contribute to low libido symptoms, making it difficult to focus on sexual connection. Relationship dynamics, including emotional disconnection, unresolved conflicts, or lack of intimacy, can also impact desire. If you're experiencing low sex drive, it's essential to seek a low libido diagnosis from a healthcare provider. A doctor can assess possible underlying causes, including hormonal imbalances, medical conditions, or medication side effects. Fortunately, various low libido treatment options exist, including hormone therapy, counselling, lifestyle changes, and stress management techniques. Open communication with your partner and healthcare provider can help create a supportive environment to address concerns and improve overall well-being. By understanding the root causes and exploring solutions, many women can restore their sexual desire and enhance intimacy. Birth control and low libido Hormonal birth control methods, such as the pill, patch, or implant, can affect libido by altering hormone levels in the body. These changes might lead to a decrease in sex drive for some individuals. For example, a woman who starts using the birth control pill may notice a decline in her desire for sex. This is because the pill can lower levels of testosterone, a hormone that plays a role in sexual desire. Low libido in men Low libido is a common issue among men, with around 15% to 16% of men reporting a persistent lack of sexual desire. Low sex drive in men can be influenced by various factors, including: Stress, anxiety, and depression Relationship issues Physical health conditions like erectile dysfunction Certain medications Lifestyle choices such as excessive alcohol consumption Additionally, hormonal imbalances, especially those related to testosterone levels, may play a role in low libido in men. Testosterone is a key hormone that regulates sexual desire in males. As men age, their testosterone levels naturally decline, which can contribute to a decrease in libido. How is low libido diagnosed? Low libido diagnosis involves identifying the underlying causes, which can include medical conditions, psychological factors, or lifestyle influences. A healthcare provider will typically conduct a thorough medical and psychological evaluation to determine the reasons for reduced sex drive. During the diagnostic process, your doctor may: Discuss your medical history, including any chronic conditions or medications you're taking Ask about your mental health, such as whether you're experiencing stress, anxiety, or depression Inquire about your relationship status and any concerns related to your partner Order blood tests to check hormone levels and rule out underlying health issues Providing honest and open answers to your healthcare provider's questions can help them accurately diagnose the cause of your low libido. How is low libido treated? Low libido treatment depends on the underlying cause, and a comprehensive approach is often necessary to restore sexual desire. Several effective strategies can help individuals address and overcome low sex drive. For those experiencing relationship difficulties, couples therapy or relationship counseling can improve communication and emotional intimacy, which may enhance sexual desire. Medical interventions are another option. Medication such as Viagra or Cialis may be prescribed for men with erectile dysfunction, while women with hypoactive sexual desire disorder (HSDD) may benefit from medications like Addyi (flibanserin). In cases where hormonal imbalances are responsible, hormone replacement therapy (HRT), such as testosterone therapy for men or estrogen therapy for menopausal women, may be recommended. Psychotherapy, including cognitive-behavioral therapy (CBT) or sex therapy, can help individuals address psychological factors such as stress, anxiety, or negative beliefs about sex. For men wondering how to increase libido in men, lifestyle adjustments are crucial. Regular exercise, proper sleep, stress reduction, and limiting alcohol intake can all contribute to improved libido. A thorough low libido diagnosis from a healthcare provider can help identify the best course of action, ensuring a tailored approach to restoring sexual desire. What can we do if we have low libido? If you're experiencing low sex drive, try open communication with your partner, stress-reduction techniques like meditation or yoga, and regular physical activity to boost mood and energy. Limit alcohol, quit smoking, and prioritise self-care. Foster emotional intimacy through shared activities. If needed, consult a healthcare provider to address underlying medical or psychological causes. When should I see a doctor about low libido? You should consult a doctor about low libido if your lack of sexual desire persists for several weeks or months, especially if it causes distress or relationship issues. If you suspect an underlying health condition or medication side effect is affecting your libido, seeking medical advice is essential. Additionally, experiencing other symptoms like pain during sex or difficulty getting aroused may indicate an underlying issue that requires professional evaluation. Conclusion Low libido is a complex issue that can stem from a variety of biological, psychological, and social factors. Understanding the cause is crucial for effective low libido treatment. If you're concerned about low libido, consider reaching out to Metropolis Healthcare for diagnostic testing and health check-ups. Their team of qualified blood collection technicians can make at-home visits for blood samples, which are processed at state-of-the-art labs. Test reports are conveniently shared online, empowering you to take charge of your health.
Vulvar Cancer: Symptoms, Causes, and Risk Factors
What is Vulvar Cancer? Vulvar cancer is a rare type of cancer that develops in the outer part of the female genitals. While it most commonly affects older women over 65, it's important for women of all ages to be aware of the signs and risk factors. Early detection greatly improves treatment outcomes, so recognising symptoms like persistent itching, skin changes, and unusual bleeding is crucial. Although the exact causes are unknown, factors like human papillomavirus (HPV) infection and smoking can increase risk. Understanding the warning signs and risk factors can help you take proactive steps towards prevention and timely intervention. Vulvar cancer develops in the tissues of the vulva, which include the labia, clitoris, and the opening of the vagina. Squamous cell carcinoma, arising from the skin cells of the vulva, accounts for about 90% of vulvar cancers. While vulvar cancer is uncommon, representing about 4% of gynaecological cancers, its incidence is gradually increasing, especially in younger women. The exact cause of vulvar cancer is not clear, but various factors can increase a woman's risk. Early detection is crucial, as it significantly improves the chances of successful treatment. Being aware of the signs and symptoms and reporting any unusual changes to your doctor can help catch vulvar cancer at an early stage. Symptoms of Vulvar Cancer Vulvar cancer symptoms can be similar to those of other, less serious conditions. However, if you experience any of the following persistently, it's important to consult your doctor: Persistent itching, burning, or soreness in the vulva Thickened, discolored, or rough patches on the vulvar skin Appearance of lumps, warts, or ulcers on the vulva Unusual vaginal bleeding or discharge, especially after menopause Pain or discomfort during urination or sexual intercourse Changes in the appearance of a mole or freckle on the vulva Swelling in the vulvar area or groin lymph nodes These symptoms don't necessarily mean you have vulvar cancer, as they can be caused by other conditions like infections. However, it's crucial not to ignore persistent symptoms. If you notice any unusual changes or symptoms lasting more than two weeks, make an appointment with your gynaecologist. Causes and Risk Factors of Vulvar Cancer While the exact vulvar cancer causes are unknown, certain factors can increase a woman's risk: Human Papillomavirus (HPV) Infection: Exposure to high-risk HPV strains, especially HPV 16, increases vulvar cancer risk. However, HPV is very common, and most women with HPV do not develop vulvar cancer. Age: The risk of vulvar cancer increases with age, with over half of cases diagnosed in women older than 70. However, vulvar cancer is becoming more common in younger women. Smoking: Cigarette smoking doubles vulvar cancer risk, likely because tobacco chemicals damage vulvar skin cells. Weakened Immune System: Conditions or medications that suppress the immune system, such as HIV or prolonged steroid use, can increase risk. Skin Conditions: Chronic inflammatory skin conditions of the vulva, like lichen sclerosus, are associated with a slightly elevated vulvar cancer risk. Precancerous Conditions: Vulvar intraepithelial neoplasia (VIN), where vulvar skin cells develop abnormally, can potentially progress to cancer if untreated. Having one or more of these risk factors doesn't mean you'll definitely develop vulvar cancer. However, it's important to be aware of them so you can take steps to reduce your risk where possible and stay vigilant about any potential symptoms. Diagnosis of Vulvar Cancer If your doctor suspects vulvar cancer based on your symptoms and physical exam, they will recommend tests to confirm the diagnosis: Medical History and Physical Exam: The doctor takes a detailed medical history and conducts a pelvic exam to check for lumps, skin changes, or other abnormalities. Colposcopy: A colposcope magnifies the vulva to inspect suspicious areas, which may be treated with acetic acid or toluidine blue for better visibility. Biopsy: A tissue sample is taken from the suspicious area and examined under a microscope to confirm cancer. Imaging Tests: If cancer is confirmed, imaging tests like CT scans, MRIs, or PET scans are used to check for spread to other parts of the body. Staging: The cancer is staged from stage 1 (localised) to stage 4 (spread to distant areas), helping guide treatment decisions. Your doctor may also recommend additional tests based on your individual situation. Treatment Options for Vulvar Cancer Vulvar cancer treatment depends on various factors, including the cancer stage, type, and location, as well as your overall health and preferences. The main treatment modalities are: Surgery: The primary treatment for most vulvar cancers is surgical removal of the tumor and a margin of surrounding healthy tissue. In some cases, nearby lymph nodes are also removed. The extent and impact of surgery depend on the cancer's size and spread. Radiation Therapy: High-energy radiation beams are used to kill cancer cells. It may be used before surgery to shrink tumors, after surgery to destroy remaining cancer cells, or as the main treatment if surgery isn't possible. Chemotherapy: Cancer-fighting medicines are administered orally or intravenously to kill cancer cells throughout the body. Chemotherapy is mainly used for advanced vulvar cancers or in combination with radiation. Topical Therapy: For precancerous vulvar changes or very early superficial vulvar cancers, topical medications may be applied directly on the skin. In many cases, a combination of these treatments offers the best outcome. Your cancer care team will work with you to develop a personalised treatment plan tailored to your specific situation. Living with Vulvar Cancer A vulvar cancer diagnosis can feel overwhelming, affecting your physical, emotional, and sexual well-being. Coping with treatment side effects, changes in body image, and intimacy concerns can be challenging. It's crucial to prioritise self-care and reach out for support: Follow your treatment plan diligently and keep all follow-up appointments Communicate openly with your healthcare team about any side effects or concerns Practice healthy lifestyle habits to support your body during treatment and recovery Consider joining a vulvar cancer support group to connect with others who understand Seek counseling or therapy to process the emotional impact of cancer Explore options like pelvic floor physiotherapy to manage physical discomfort Be patient and compassionate with yourself as you navigate this journey Prevention and Early Detection While there's no guaranteed way to prevent vulvar cancer, certain steps may lower your risk: Practicing safe sex and limiting sexual partners to reduce HPV exposure Quitting smoking, as tobacco use is linked to increased risk Attending regular gynecologic checkups and promptly reporting unusual symptoms Considering HPV vaccination, especially for younger women, to prevent infection with high-risk HPV strains Awareness is key—learning to recognize warning signs can help catch vulvar cancer at an early, more treatable stage. Conclusion and Key Takeaways Vulvar cancer, though uncommon, demands our attention and awareness. By familiarizing yourself with the symptoms, causes, and risk factors associated with this condition, you can be proactive in safeguarding your reproductive health. Remember, early detection is paramount to improving treatment outcomes and quality of life. If you have any concerns or notice unusual changes in your vulvar area, don't hesitate to consult with your doctor. At Metropolis Healthcare, we understand the importance of accurate diagnosis and personalised care. Our team of skilled pathologists and state-of-the-art diagnostic facilities are equipped to provide you with reliable results and support throughout your healthcare journey. Take charge of your well-being by staying informed, practicing preventive measures, and prioritising regular check-ups. Together, we can work towards better vulvar cancer awareness, early detection, and improved outcomes for women everywhere.
Whipple's Disease: Understanding Causes, Symptoms & Treatment
Whipple's disease is a rare, chronic bacterial infection that primarily affects the small intestine but can impact various systems throughout the body. First described by Dr. George Whipple in 1907, this condition is caused by the bacterium Tropheryma whipplei and can lead to a wide range of symptoms, including digestive issues, joint pain, and neurological problems. Despite its rarity, Whipple's disease can be life-threatening if left untreated. In this article, we'll delve into the causes, risk factors, Whipple's disease symptoms, diagnostic methods, treatment options, and long-term management strategies to help you better understand this complex condition. What is Whipple's Disease? Whipple's disease is a systemic infectious disease caused by the bacterium Tropheryma whipplei. This bacteria primarily infects the small intestine, damaging the villi, which are tiny finger-like projections that absorb nutrients. As a result, people with Whipple's disease often experience malabsorption, leading to malnutrition and a range of gastrointestinal symptoms. However, the infection can spread to other parts of the body, such as the heart, lungs, brain, and eyes, causing a variety of systemic symptoms. Causes and Risk Factors of Whipple's Disease Whipple's disease is caused by the bacterium Tropheryma whipplei, which infects the mucosal lining of the small intestine, leading to nutrient malabsorption. The bacterium disrupts immune system function, causing inflammation in multiple organs, including the intestines, joints, heart, and nervous system. The exact mechanism of how T. whipplei causes the disease is still not fully understood, but it involves the bacterium persisting within immune cells (macrophages) and spreading throughout the body. Risk factors for developing Whipple's disease include: Age: Most commonly affects individuals between 40 and 60 years old. Gender: Men are more frequently affected than women. Ethnicity: More common in white individuals, particularly in North America and Europe. Occupation: Outdoor workers, such as farmers, may have a higher risk due to exposure to contaminated soil and water. Immune System Dysfunction: Individuals with weakened immune systems, such as those with HIV/AIDS or organ transplant recipients, are at greater risk. Genetic Factors: Genetic variations may increase susceptibility, though specific genes have not been identified. Symptoms of Whipple's Disease The signs and symptoms of Whipple's disease can vary widely and often mimic those of other conditions, making diagnosis challenging. Some common Whipple's disease symptoms include: Digestive Issues: Diarrhea Abdominal pain and cramping Weight loss Malnutrition Joint Problems: Joint pain (arthralgia) Swelling and stiffness in the joints Neurological Symptoms: Memory loss and confusion Vision changes Difficulty with muscle coordination Other Potential Symptoms: Chronic cough Fever Anemia Skin darkening or hyperpigmentation How is Whipple's Disease Diagnosed? Diagnosing Whipple's disease often involves a combination of clinical evaluation, laboratory tests, and imaging studies. These include: Medical History and Physical Exam: Your doctor will ask about your symptoms, medical history, and potential risk factors. They will also perform a thorough physical examination to check for signs like abdominal tenderness, joint swelling, or skin changes. Blood Tests: Blood work may be ordered to assess your overall health, check for nutritional deficiencies, and rule out other potential causes of your symptoms. Endoscopy and Biopsy: An upper endoscopy procedure allows your doctor to visualise your digestive tract and obtain tissue samples (biopsy) from your small intestine. These samples are then examined under a microscope to look for the presence of T. whipplei bacteria. Polymerase Chain Reaction (PCR) Testing: This sensitive test can detect the DNA of T. whipplei in tissue or fluid samples, aiding in the diagnosis of Whipple's disease. Treatment Options for Whipple's Disease Prompt and effective treatment is crucial for managing Whipple's disease and preventing serious complications. The primary treatment approach involves: Initial Antibiotic Course: Treatment typically begins with a 2-4 week course of intravenous antibiotics, such as ceftriaxone or penicillin, to quickly reduce the bacterial load. Long-Term Oral Antibiotics: Following the initial IV treatment, you will need to take oral antibiotics, usually trimethoprim-sulfamethoxazole (TMP-SMX), for an extended period, often 1-2 years, to eliminate any remaining bacteria and prevent relapse. Nutritional Support: Your doctor may recommend dietary changes and nutritional supplements to address any malnutrition or vitamin deficiencies resulting from malabsorption. Monitoring and Follow-Up: Regular check-ups and periodic testing are essential to monitor your response to Whipple's disease treatment, assess for any complications, and ensure the infection has been fully eradicated. Complications and Long-Term Outlook If left untreated, Whipple's disease can lead to serious, potentially life-threatening complications, such as: Severe malnutrition and weight loss Neurological damage, including dementia and seizures Heart valve damage (endocarditis) Eye inflammation and vision loss However, with prompt diagnosis and appropriate antibiotic treatment, the majority of people with Whipple's disease can achieve a full recovery. It's important to note that relapses can occur, so ongoing monitoring and follow-up care are crucial. Prevention and Management Strategies As the exact cause of Whipple's disease is not well understood, there are no specific prevention strategies. However, some general measures may help reduce the risk of infection: Maintain good hygiene practices, especially when working with soil or wastewater Boost your immune system through a healthy diet, regular exercise, and stress management Seek prompt medical attention if you experience persistent gastrointestinal, joint, or neurological symptoms For those diagnosed with Whipple's disease, adhering to the prescribed antibiotic regimen and attending regular follow-up appointments are crucial for successful treatment and preventing relapse. When to See a Doctor Here are situations when you should consult a doctor: Persistent Symptoms: Ongoing gastrointestinal issues such as chronic diarrhea, abdominal pain, and unexplained weight loss, especially if worsening over time. Joint Pain: Unresolved joint pain, especially if accompanied by other symptoms like fever or fatigue. Neurological Symptoms: Immediate medical care is needed if you experience confusion, memory loss, seizures, or vision problems, as these may indicate central nervous system involvement. Skin Changes: Any unusual skin changes, such as dark spots, should be evaluated by a healthcare professional. Nutritional Deficiencies: Symptoms like extreme fatigue, weakness, or signs of anemia (such as pallor or shortness of breath) require a doctor's visit. Family History: If there is a family history of bowel disorders or similar symptoms in close contacts, it’s wise to consult a doctor. Conclusion and Key Takeaways Whipple's disease is a rare but serious bacterial infection that can affect multiple systems in the body. Prompt diagnosis and long-term antibiotic treatment are essential for managing the condition and preventing complications. If you suspect you may have Whipple's disease or are experiencing persistent gastrointestinal, joint, or neurological symptoms, don't hesitate to seek medical attention. Metropolis Healthcare, a leading chain of diagnostic labs across India, offers comprehensive pathology testing services to help diagnose and monitor various health conditions, including Whipple's disease. With a team of qualified blood collection technicians and state-of-the-art diagnostic labs, we are committed to delivering accurate results and personalised care to empower patients in prioritising their health.
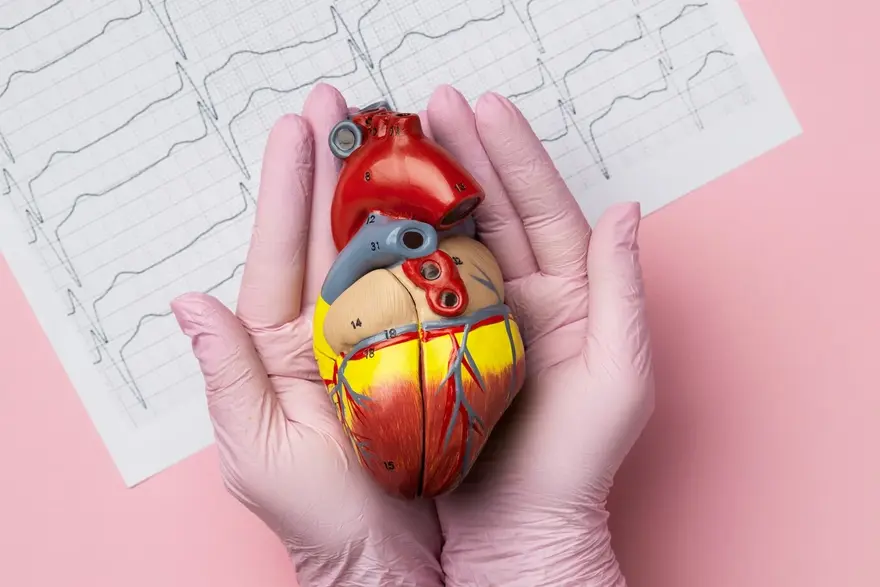
Ventricular Fibrillation: Causes, Symptoms, and Risk Factors Explained
What is Ventricular Fibrillation? Ventricular fibrillation is a life-threatening heart rhythm disorder that requires immediate medical attention. This condition occurs when the heart's lower chambers (ventricles) quiver chaotically, disrupting the heart's ability to pump blood effectively throughout the body. Without prompt treatment, ventricular fibrillation can lead to sudden cardiac arrest and death. Understanding the causes, symptoms, and risk factors associated with this serious arrhythmia is crucial for timely intervention and potentially saving lives. In this article, we will explore the key aspects of ventricular fibrillation, helping you stay informed and prepared. How Does Ventricular Fibrillation Differ from Other Arrhythmias? While there are many types of heart rhythm disorders, ventricular fibrillation stands out due to its life-threatening nature. In ventricular fibrillation, the heart's electrical signals become rapid and erratic, causing the ventricles to quiver ineffectively rather than contract and pump blood to the body. This chaotic rhythm prevents adequate blood circulation, leading to sudden cardiac arrest if not promptly treated with defibrillation. In contrast, other arrhythmias like atrial fibrillation or premature ventricular contractions may cause irregular heartbeats but do not always stop the heart from pumping blood altogether. Causes and Risk Factors of Ventricular Fibrillation Several factors can contribute to the ventricular fibrillation causes, including: Insufficient Blood Flow to the Heart Muscle: Blocked coronary arteries during or after a heart attack can deprive the heart muscle of oxygen, leading to ventricular fibrillation. Damage to the Heart Muscle: Conditions like cardiomyopathy or previous heart attacks can weaken the heart, increasing the risk of ventricular fibrillation due to disrupted electrical pathways. Electrolyte Imbalances: Abnormal potassium or magnesium levels can disturb the heart's electrical signals, triggering ventricular fibrillation. Drug Toxicity: Drugs like cocaine, methamphetamines, and certain medications can affect the heart’s electrical activity, contributing to ventricular fibrillation. Electrocution or Trauma: Severe physical trauma or electrocution can directly impact the heart’s electrical system, leading to ventricular fibrillation. Sepsis and Infections: Severe infections, especially sepsis, can weaken heart function and increase the risk of ventricular fibrillation. Here are the risk factors for ventricular fibrillation: Previous episodes of ventricular fibrillation Having a family history of heart disease or arrhythmias Inherited conditions such as long QT syndrome or Brugada syndrome A weakened heart muscle (cardiomyopathy) Certain medicines that affect heart function Symptoms of Ventricular Fibrillation The ventricular fibrillation symptoms can come on suddenly and may include: Sudden collapse or loss of consciousness Absence of pulse or heartbeat Gasping or not breathing Chest pain or discomfort (may occur shortly before the onset of ventricular fibrillation) Dizziness or lightheadedness Rapid or pounding heartbeat (may precede the arrhythmia) It's important to note that ventricular fibrillation often leads to cardiac arrest within seconds, so prompt recognition and medical attention are vital. Diagnosis of Ventricular Fibrillation Diagnosing ventricular fibrillation typically occurs in emergency situations and involves: Physical Examination: Doctors will assess the person's responsiveness, breathing, and circulation to determine the presence of cardiac arrest. Medical History: Information about pre-existing heart conditions, medications, and family history can help guide the diagnosis and treatment approach. Electrocardiogram (ECG or EKG): The primary diagnostic tool for ventricular fibrillation. An ECG shows rapid, erratic electrical activity with no identifiable P waves, QRS complexes, or T waves and a heart rate typically between 300-400 beats per minute. Echocardiogram: Uses ultrasound to assess the heart’s structure and function, helping to identify potential underlying heart issues contributing to ventricular fibrillation. Blood Tests: Help detect heart damage by measuring enzymes released during a heart attack, such as troponin, and can also identify electrolyte imbalances. Imaging Tests (MRI or CT scans): May be used to assess the heart’s condition and identify underlying causes, such as blockages or structural abnormalities. Rapid diagnosis is essential to initiate appropriate treatment and improve the chances of survival. Treatment Options for Ventricular Fibrillation Prompt ventricular fibrillation treatment is critical for survival. The main approaches include: Defibrillation: Delivering a controlled electric shock to the heart to reset its rhythm. This is done using an automated external defibrillator (AED) or by medical professionals. Cardiopulmonary Resuscitation (CPR): Performing chest compressions and rescue breaths to manually circulate oxygenated blood until an AED arrives or until the person can receive advanced life support measures. Medications: Administering anti-arrhythmic drugs like amiodarone or lidocaine to help stabilise the heart rhythm and prevent recurrence of ventricular fibrillation. Implantable Cardioverter Defibrillator (ICD): Surgically placing a battery-powered device under the skin to continuously monitor heart rhythms and deliver a shock if it detects ventricular fibrillation. ICDs are often recommended for people at high risk of sudden cardiac arrest. Treating Underlying Conditions: Addressing heart disorders, electrolyte imbalances, or other health issues that raise the risk of ventricular fibrillation. This may involve procedures like coronary angioplasty, heart valve surgery, or medication adjustments. The specific treatment plan depends on the individual's overall health, the cause of ventricular fibrillation, and the severity of the episode. Living with Ventricular Fibrillation: What to Expect Surviving ventricular fibrillation often requires ongoing management and lifestyle adjustments, such as: Regular check-ups to monitor heart health and adjust treatment as needed Lifestyle changes like eating a heart-healthy diet, exercising regularly, reducing stress, and avoiding tobacco and excessive alcohol Taking prescribed medications consistently to control arrhythmias and treat related conditions Learning to recognise warning signs and being prepared to respond to a cardiac emergency Wearing a medical alert bracelet and informing family, friends, and co-workers about your condition. Prevention Strategies for Ventricular Fibrillation Preventing ventricular fibrillation involves addressing risk factors and promoting heart health through: Managing underlying cardiovascular conditions, such as coronary artery disease, heart failure, and hypertension. Adopting a heart-healthy lifestyle, including a balanced diet, regular physical activity, and avoiding smoking and excessive alcohol consumption. Controlling diabetes, obesity, and other conditions that can impact heart health. Following a prescribed medication regimen and reporting any adverse effects to a doctor. Learning CPR and familiarising oneself with the ventricular fibrillation meaning and location of AEDs in frequently visited places. While not all cases of ventricular fibrillation can be prevented, these strategies can significantly lower the risk and improve overall cardiovascular well-being. Conclusion: The Importance of Awareness and Action Ventricular fibrillation is a serious and potentially life-threatening heart rhythm disorder that demands swift recognition and intervention. By understanding the causes, symptoms, and risk factors associated with this condition, individuals can be better prepared to respond effectively and seek timely ventricular fibrillation treatment. Awareness also plays a crucial role in prevention, as adopting heart-healthy habits and managing underlying cardiovascular issues can reduce the likelihood of developing ventricular fibrillation. If you or someone around you experiences symptoms suggestive of this arrhythmia, call emergency services immediately and be prepared to perform CPR if needed. If you have concerns about your heart health or wish to assess your risk factors, consider reaching out to Metropolis Healthcare. As a leading diagnostic laboratory chain in India, we offer comprehensive cardiac health check-ups and advanced blood tests to help you stay informed about your cardiovascular well-being. Our team of experienced phlebotomists can conveniently collect samples from the comfort of your home, ensuring a hassle-free experience. Take charge of your heart health today and book an appointment with Metropolis Healthcare for personalised care and reliable diagnostic services.
Peyronie's Disease: Causes, Symptoms, and Diagnosis
What is Peyronie's Disease? Peyronie's disease is a condition that affects the penis, causing abnormal curvature during erections. This can lead to pain, discomfort, and difficulties with sexual intercourse. While discussing penile health issues may feel awkward, understanding Peyronie's disease causes, symptoms, and diagnosis is crucial for seeking timely treatment and support. In this article, we'll provide a comprehensive overview of Peyronie's disease to help you navigate this challenging condition with greater awareness and confidence. Symptoms of Peyronie's Disease The symptoms of Peyronie's disease can develop gradually or appear suddenly. Some common Peyronie's disease symptoms include: Scar Tissue: You may feel flat lumps or bands of hard tissue under the skin of the penis, known as plaques. Curved Erections: Your penis may curve upward, downward, or to the side during erections due to the scar tissue. Painful Erections: You may experience penile pain, especially during erections, though this often improves over time. Erectile Dysfunction: Peyronie's disease can make it difficult to get or maintain an erection. Penile Shortening: Your penis might become shorter as a result of the condition. If you notice any of these symptoms, it's essential to consult a doctor for an accurate diagnosis and an appropriate Peyronie's disease treatment plan. Causes and Risk Factors of Peyronie's Disease While the exact cause of Peyronie's disease is not always clear, several factors can contribute to its development: Penile Injury: Trauma to the penis, such as bending or hitting, can cause bleeding and subsequent scar tissue formation. This can occur during vigorous sexual activity, sports, or accidents. Genetic Factors: Some studies suggest that certain genetic characteristics may predispose individuals to develop Peyronie's disease. Connective Tissue Disorders: People with conditions like Dupuytren's contracture, which affects the hands, appear to have a higher risk of Peyronie's disease. Age: The condition is more common in men over 50, though it can occur at any age. Other Factors: Smoking, certain medications, and health conditions like diabetes might increase the likelihood of developing Peyronie's disease. Understanding these risk factors can help you take steps to minimise your chances of developing the condition or worsening existing symptoms. Diagnosis of Peyronie's Disease To diagnose Peyronie's disease, your doctor will typically: Medical History: The doctor will ask about the patient’s symptoms, including when they first noticed a curvature, pain during erections, or difficulty with sexual activity. They may also ask about any history of trauma or injury to the penis. Physical Examination: A physical exam is performed, typically when the penis is flaccid and, in some cases, during an erection, to assess the degree and location of the curvature or deformity. The doctor will also check for lumps or plaques under the skin. Ultrasound: A common diagnostic tool is ultrasound, which can evaluate the size, location, and consistency of the plaque and assess blood flow to the penis. X-rays or MRI: In some cases, imaging techniques like MRI or X-rays may be used if the doctor needs more detailed information about the extent of the disease. Erection Induction: In some cases, doctors may use medications (such as prostaglandin E1) to induce an erection in a controlled setting so they can evaluate the curvature and the impact of the disease on erectile function. Assessment of Erectile Function: Since Peyronie's disease often affects erectile function, the doctor may ask questions related to erectile dysfunction or perform tests to assess blood flow and the ability to maintain an erection. Treatment Options for Peyronie's Disease Treatment for Peyronie's disease depends on the severity of symptoms and the stage of the condition. Some Peyronie's disease treatment options include: Watchful Waiting: If your symptoms are mild and not causing significant problems, your doctor may recommend monitoring the condition over time to see if it improves on its own. Medications: Oral medications like pentoxifylline or colchicine may help reduce inflammation and slow the progression of scar tissue. Injections of medications directly into the scar tissue, such as verapamil or interferon, can also be used to reduce plaque size and curvature. Medical Therapies: Techniques like iontophoresis (using an electric current to deliver medication through the skin) or extracorporeal shockwave therapy (using sound waves to break up scar tissue) may be recommended in some cases. Surgery: For severe cases that don't respond to other treatments, surgery may be necessary. Options include removing scar tissue, placing grafts or implants to straighten the penis, or implanting penile prostheses to help with erections. Penile Traction Therapy: A non-invasive method that uses a device to gently stretch the penis over time, potentially reducing curvature and improving length. It is most effective with consistent use over several months. Your doctor will work with you to determine the most appropriate Peyronie's disease treatment plan based on your individual needs and goals. Living with Peyronie's Disease Coping with Peyronie's disease can be challenging, both physically and emotionally. Some strategies that may help include: Communicating openly with your partner about your condition and how it affects your sexual function and intimacy. Seeking support from a therapist or counselor to address feelings of anxiety, depression, or low self-esteem related to the condition. Practicing stress-reduction techniques like deep breathing, meditation, or gentle exercise to manage emotional distress. Maintaining a healthy lifestyle through a balanced diet, regular physical activity, and avoiding smoking and excessive alcohol consumption. Prevention and Early Intervention While there is no guaranteed way to prevent Peyronie's disease, there are steps you can take to reduce your risk and catch the condition early: Practice safe sex techniques to avoid injury to the penis. Maintain good overall health by eating a balanced diet, exercising regularly, and managing stress. Be aware of the early signs and symptoms of Peyronie's disease, like penile pain, curvature, or lumps. Schedule regular check-ups with your doctor, especially if you have a family history or other risk factors for the condition. Early diagnosis and treatment can help prevent the condition from worsening and improve long-term outcomes. If you notice any concerning symptoms, don't hesitate to seek medical advice. Conclusion and Key Takeaways Peyronie's disease is a condition characterised by the development of scar tissue in the penis, leading to curvature, pain, and sexual difficulties. By understanding the Peyronie's disease causes, symptoms, and diagnostic process, you can take an active role in managing your health and seeking appropriate treatment. If you are experiencing symptoms of this condition, don't hesitate to consult with a doctor for a detailed Peyronie's disease treatment plan. Metropolis Healthcare offers comprehensive diagnostic services, including at-home sample collection, to help you get the answers and care you need. With the right support and treatment plan, it is possible to manage Peyronie's disease and maintain a healthy, fulfilling life.













 WhatsApp
WhatsApp