Preventive Healthcare
Understanding Osteomyelitis (Bone Infection): Symptoms, Causes, and Treatment
2467 Views
0
What is osteomyelitis?
Osteomyelitis is the inflammation or swelling of bone tissue, typically arising from an infection. It can occur when infections enter the bone through the bloodstream, spread from nearby tissues, or originate within the bone itself due to exposure to germs following an injury.
How common is osteomyelitis?
The occurrence of osteomyelitis varies depending on the age group and the specific category of the disease. In the case of hematogenous spread, which is the predominant type in children, the United States reports an estimated 2-5 cases per 10,000 people, with a potentially higher incidence in developing nations.
Who might have osteomyelitis?
People with weak immune systems, such as those with conditions like sickle cell disease or HIV, or individuals undergoing immunosuppressive treatments like chemotherapy or steroids, have a higher susceptibility to the development of bone infection or osteomyelitis.
What are the types of osteomyelitis?
The following are osteomyelitis types, reported commonly-
- Acute
This form of osteomyelitis manifests suddenly, often accompanied by a fever, followed by the onset of pain in the affected area a few days later.
- Chronic
- Chronic osteomyelitis is characterised by a persistent bone infection that does not respond to conventional treatments.
- Symptoms include ongoing bone pain and recurrent drainage of pus.
- In some cases, chronic osteomyelitis may be asymptomatic, remaining undetected for months or even years.
- Vertebral
- This type of bone infection specifically targets the spine, leading to chronic back pain that exacerbates with movement.
- Traditional remedies such as rest, heat therapy, and pain relievers may not provide relief.
- It seldom induces fever and is more prevalent among individuals in nursing homes, those who misuse intravenous drugs, or individuals undergoing dialysis.
What causes osteomyelitis?
- Osteomyelitis involves incidences where bacteria from nearby infected tissue or an open wound enter the bloodstream and settle in bone, where they proliferate.
- Staphylococcus aureus bacteria, commonly associated with staph infections, are a primary osteomyelitis cause. In some cases, a bone infection may be caused by a fungus or other types of germs.
Causes of osteomyelitis may include:
- Artificial joint, such as a hip replacement
- Blood infection or conditions like sickle cell anaemia
- Diabetes, particularly in cases of diabetes-related foot ulcers
- Metal implants in bone, such as screws
- Pressure injuries are commonly known as bedsores
- Recent broken bone or bone surgery
- Traumatic injury or wound
- Weakened immune system
What are the symptoms of osteomyelitis?
One of the initial osteomyelitis symptoms that often emerge is pain at the site of infection. Additional common osteomyelitis symptoms include:
- Fever and chills
- Redness in the infected area
- Irritability or a general feeling of being unwell
- Drainage from the affected area
- Swelling in the impacted region
- Stiffness or an inability to use the affected limb
How is osteomyelitis diagnosed?
- Diagnosis of a potential bone infection involves a comprehensive approach, with the doctor conducting a physical examination to assess swelling, pain, and discolouration.
- Lab and diagnostic tests are often ordered to precisely locate and gauge the extent of the infection.
- Blood tests are commonly employed to identify the organisms causing the infection, while additional tests such as throat swabs, urine cultures, and stool analyses may also be conducted.
- A stool culture, which is a type of stool analysis, might be performed.
- A bone scan is another diagnostic method, revealing cellular and metabolic activity in the bones using a radioactive substance to highlight bone tissue. If more detailed information is needed, an MRI scan may be recommended.
- In some instances, a bone biopsy might be necessary for a definitive osteomyelitis diagnosis.
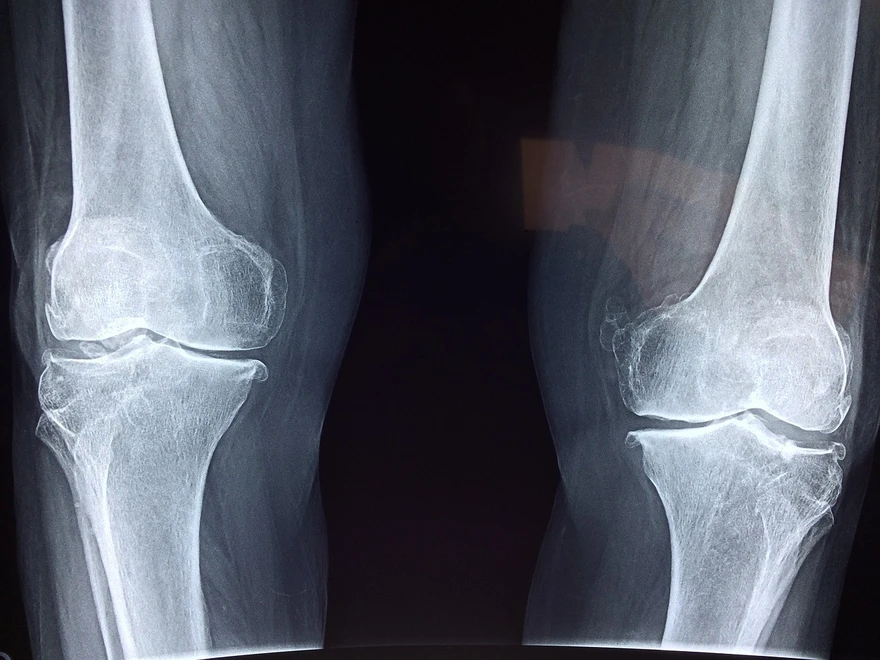
- Despite these advanced tests, a simple bone X-ray can sometimes be sufficient for the doctor to determine an appropriate treatment plan for bone infection.
What are the complications of osteomyelitis?
Complications associated with osteomyelitis include:
- Bone abscess: Formation of a pocket of pus within the bone
- Bone necrosis: Death of bone tissue
- Spread of infection to surrounding areas
- Inflammation of soft tissue (cellulitis)
- Blood poisoning (septicaemia)
- Chronic infection that proves resistant to treatment
How is osteomyelitis managed or treated?
Common osteomyelitis treatment typically involves a combination of surgical intervention and intravenous antibiotic therapy administered in a hospital setting.
Surgery for osteomyelitis:
- Drain the infected area: Opening up the infected bone area allows for the drainage of accumulated pus or fluid in response to the infection.
- Remove diseased bone and tissue (debridement): This osteomyelitis treatment involves the removal of as much diseased bone as possible, ensuring a small margin of healthy bone is taken to eliminate all infected areas.
- Restore blood flow to the bone: Surgeons may use a piece of bone or other tissue from another part of the body to fill any void left by debridement. Temporary fillers may be used until the patient is healthy enough for a bone or tissue graft, promoting the repair of damaged blood vessels and new bone formation.
- Remove foreign objects: Surgical plates or screws from previous surgeries may need extraction in certain cases.
- Amputate the limb: In extreme cases, limb amputation may be considered as a last resort to halt the spread of infection for osteomyelitis treatment.
Medications for osteomyelitis:
- Antibiotics: Determined through a bone biopsy, antibiotics are administered intravenously for approximately six weeks, with additional oral antibiotics for more severe infections.
- Smoking cessation and chronic condition management: Quitting smoking aids in faster healing, and managing underlying chronic conditions, such as diabetes, is crucial for recovery.
How can you prevent osteomyelitis?
Preventive Measures:
- Avoiding Injected Illegal Drugs: Refrain from engaging in the use of injected illegal substances to reduce the risk of osteomyelitis.
- Prompt Medical Care for Diabetes: If you have diabetes, ensure timely medical attention for any foot-related issues to minimise the likelihood of osteomyelitis.
- Wearing Shoes for Peripheral Neuropathy: If you experience peripheral neuropathy, always wear shoes to prevent wounds, a crucial step in osteomyelitis prevention.
What is the outlook for osteomyelitis?
The prognosis for chronic osteomyelitis is less optimistic, with symptoms persisting for years, even after surgery. In some cases, amputation may be necessary, particularly for individuals with diabetes or compromised blood circulation.
Prognosis for Prosthetic Infections:
Influencing Factors: The outlook for individuals with a prosthesis infection is influenced by:
- Person's Health
- Type of Infection
- Feasibility of Prosthesis Removal
When to see a doctor?
Seek medical attention if you develop osteomyelitis symptoms or if the condition persists despite treatment.
Conclusion
In conclusion, osteomyelitis, though manageable with prompt and appropriate treatment, can pose significant challenges, particularly in chronic cases. The importance of knowing osteomyelitis causes, early medical intervention for osteomyelitis symptoms and ongoing monitoring during osteomyelitis treatment cannot be overstated. With advancements in medical care and vigilant management, individuals can improve their outcomes, emphasising the crucial role of both patients and healthcare providers in addressing this bone infection.
Metropolis Healthcare, India's top pathology lab and diagnostic centre, offers a complete range of blood tests and diagnostic services, including those for osteomyelitis. Try it for timely and accurate results!























 WhatsApp
WhatsApp