Preventive Healthcare
Understanding Mucormycosis: A Rare Fungal Infection
3319 Views
0
Mucormycosis, also known as Black Fungus, is a rare yet severe fungal infection caused by mucoromycetes moulds. Amid the COVID-19 pandemic, it has gained prominence as a potential complication. This article delves into the origins, symptoms, diagnosis, and treatment of this formidable infection, offering crucial insights into understanding and managing the threat mucormycosis disease poses to health.
What is Mucormycosis?
Mucormycosis, an opportunistic fungal infection, stems from the zygomycete family, causing diverse infections. Triggered by moulds known as mucormycetes, this rare but severe condition manifests in various syndromes, especially affecting immunocompromised and diabetic individuals. Characterised by angioinvasion, tissue necrosis, and infarction, mucormycosis poses a high mortality risk. Therefore, early diagnosis and intervention are crucial for managing this invasive mycotic infection.
Who is at Risk of Developing Mucormycosis?
Mucormycosis primarily affects individuals with compromised immune systems. Understanding these risk factors is crucial for early identification and management of mucormycosis disease. Some of the vulnerable people include:
- Immunocompromised Status: Those with weakened immune defences, such as transplant recipients, cancer patients undergoing chemotherapy, and individuals with HIV/AIDS, face a higher risk.
- Diabetes Mellitus: Diabetic patients are sensitive, particularly those with poorly controlled blood sugar levels. After all, hyperglycemia provides an ideal environment for mucormycetes to thrive.
- Organ Transplants: Recipients of solid organ transplants or hematopoietic stem cell transplants are at increased risk due to immunosuppressive medications.
- Steroid Use: Prolonged or high-dose steroid therapy, common in conditions like asthma or autoimmune disorders, can compromise the immune system.
- Iron Overload: Conditions causing elevated iron levels, such as certain blood disorders or repeated blood transfusions, create a conducive environment for mucormycosis.
- Trauma or Injury: Open wounds or surgical sites provide entry points for the fungi.
- Malnutrition: Poor nutritional status weakens the immune system, increasing vulnerability.
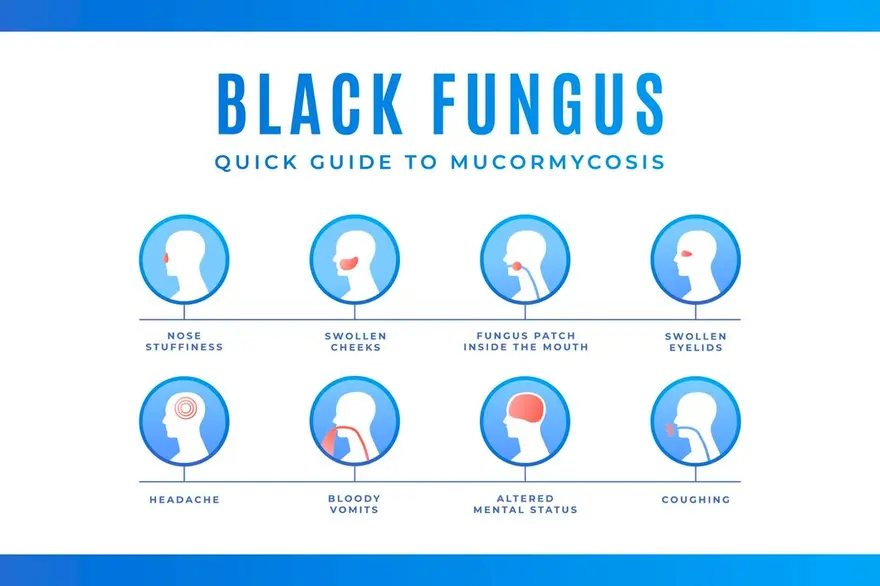
What are the Symptoms of Black Fungus (Mucormycosis)?
Mucormycosis presents with various symptoms, including:
- One-sided Facial Swelling: Notable swelling on one side of the face.
- Headache: Persistent and often severe headaches.
- Nasal or Sinus Congestion: Difficulty breathing due to nasal or sinus blockage.
- Black Lesions: Dark lesions on the nasal bridge or inside the mouth.
- Fever: Elevated body temperature.
Recognising these mucormycosis disease signs is crucial to facilitate early diagnosis and prompt treatment, especially for individuals at higher risk.
What are the Causes of Mucormycosis (Black Fungus)?
Mucormycosis arises from the opportunistic fungal infection of mucormycetes, with specific causes including:
- Zygomycetes Family Infection: Mucormycosis is primarily caused by fungi from the zygomycete family. This family includes various genera like Mucor, Rhizomucor, Cunninghamella, and more.
- Immunocompromised Conditions: Weakened immune systems, a common factor in transplant recipients, cancer patients, and those with HIV/AIDS, create an environment conducive to mucormycetes growth and invasion.
- Diabetes Mellitus: Poorly controlled diabetes provides an ideal setting for mucormycosis development, as elevated blood sugar levels promote fungal growth.
- Iron Overload: Conditions leading to elevated iron levels, like repeated blood transfusions, hemochromatosis, or certain blood disorders, create a favourable environment for mucormycetes proliferation.
- Steroid Therapy: Prolonged or high-dose steroid use, common in asthma and autoimmune disorders, weakens the immune system, making individuals more susceptible to mucormycosis.
- Trauma or Injury: Open wounds or surgical sites provide entry points for mucormycetes, leading to infection.
Understanding these mucormycosis causes is vital, especially for individuals with underlying health conditions.
How is Mucormycosis Diagnosed?
Mucormycosis is diagnosed through clinical evaluation, imaging studies, and laboratory tests.
- Clinical symptoms include necrotic tissue, fever, and facial pain. Imaging methods like CT or MRI help identify fungal invasion.
- Definitive diagnosis relies on obtaining samples via biopsy or cultures. While the tissue biopsy, commonly from affected areas like sinuses, lungs, or skin, provides direct evidence of mucormycetes, cultures, on the other hand, isolate and identify the specific fungi involved.
- Utilising molecular tests like Polymerase Chain Reaction (PCR) allows for swift identification of Mucormycosis, facilitating a quicker and more accurate diagnosis by detecting specific genetic material associated with the infection.
Can Mucormycosis Cause Other Conditions to Develop?
Mucormycosis itself is a severe fungal infection and can lead to various complications, including brain infarction, hematoma after haemorrhage, and skin ulcers. Severe cases may result in osteomyelitis and cranial nerve palsies and, if untreated, can be fatal, underlining the significance of early diagnosis and mucormycosis treatment.
What are the Treatment Options for Mucormycosis?
Mucormycosis requires a multifaceted approach for effective treatment. The key options include:
- Antifungal Medications: Prompt administration of intravenous antifungal agents, such as amphotericin B, is crucial for controlling fungal growth.
- Surgical Debridement: Surgical removal of infected tissue is often necessary, especially in sinuses or skin cases.
- Control Underlying Conditions: Managing predisposing factors like diabetes or immunosuppression is vital to prevent recurrence.
- Hyperbaric Oxygen Therapy: Some cases may benefit from adjunctive hyperbaric oxygen therapy to enhance tissue oxygenation.
- Continued Monitoring: Regular imaging and clinical assessments ensure treatment efficacy and guide further interventions.
Early detection and a coordinated approach are essential for successful mucormycosis management.
Are There Any Preventive Measures for Mucormycosis?
Indeed, there are! Preventing mucormycosis involves simple yet crucial steps:
- Hygiene Practices: Maintain good personal hygiene by regularly washing hands and changing clothes, particularly in dusty environments.
- Protective Measures: Use face masks in dusty areas, avoid water-damaged buildings and protect the skin from soil exposure.
- Early Diagnosis: Timely identification of predisposing factors and early medical intervention can significantly reduce the risk.
Adhering to these preventive measures is especially crucial for individuals with weakened immune systems.
Can Mucormycosis be Fatal?
Yes, mucormycosis can be fatal, particularly if not promptly diagnosed and treated.
The infection, often aggressive, can spread rapidly and affect vital organs. Moreover, individuals with weakened immune systems, diabetes, or other underlying health conditions are at higher risk. Therefore, early medical intervention, including antifungal medications and surgical removal of infected tissue, is crucial for improving outcomes.
Is Mucormycosis Contagious?
No, mucormycosis is not contagious. It does not spread between people or from animals to people. The fungus causing mucormycosis is found in the environment, and transmission occurs through contact with the fungal spores in the environment, not through person-to-person contact.
Is it Possible to Prevent a Mucormycosis Infection?
Preventing mucormycosis disease involves:
- Avoiding activities in dusty environments,
- Steering clear of water-damaged buildings, and
- Practising good hygiene
So, yes, it can be prevented, provided individuals with weakened immune systems should take extra precautions to minimise environmental exposure to fungal spores.
Are There Any Long-Term Effects of Mucormycosis?
Mucormycosis can lead to severe long-term consequences, including cognitive impairments, hearing loss, and necrotising fasciitis. Moreover, it can also cause intracerebral abscess complications, which is quite rare, though emphasising the potential for lasting neurological and functional impacts.
Conclusion
Mucormycosis, an emerging fungal infection primarily affecting immunocompromised individuals, poses a significant threat due to its aggressive nature and high mortality rates with standard therapy. The disease's pathogenesis remains complex and varied, contributing to its challenging management. Therefore, understanding its epidemiology, clinical manifestations, and risk factors is crucial in combating this serious and potentially fatal infection. From mucormycosis causes to symptoms and mucormycosis treatments to preventive measures, this article has been your guide. Remember, awareness is the first step towards protection. Stay informed, prioritise your health and consult doctors for guidance. For reliable diagnostic services, consider Metropolis Labs, a trusted partner in ensuring accurate and timely medical assessments.






















 WhatsApp
WhatsApp