Preventive Healthcare
Understanding Hiatal Hernia: Symptoms, Causes, and Treatment Strategies!
1420 Views
0
Introduction:
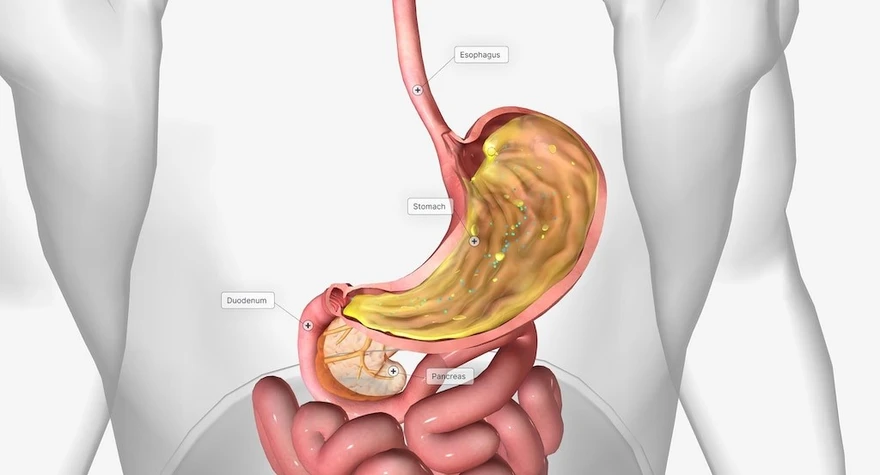
Hiatal hernia—a condition that affects millions worldwide, often without them even realising it. Picture this: a small opening in the diaphragm allowing a portion of the stomach to slowly move into the chest cavity. It's a common occurrence, especially as we age, yet its impact can be profound.
While some experience no symptoms, others grapple with acid reflux, chest pain, and difficulty swallowing, among other discomforts. In this article, we'll journey through the intricacies of hiatal hernia, shedding light on its symptoms, causes, and treatment options, empowering you to navigate this condition with knowledge and confidence.
What is a Hiatal Hernia?
A hiatal hernia happens when the part of your stomach pushes through the weak spot or opening in your diaphragm into the chest cavity. The diaphragm is a muscle barrier that separates your abdominal cavity from your chest cavity.
What are the Different Hiatal Hernia Types?
Hiatal hernias can be categorised into two main types: sliding hiatal hernia and paraoesophagheal hiatal hernia. Let's explore each hiatal hernia types in detail:
- Sliding Hiatal Hernia:
- This is the most common hiatal hernia type, accounting for around 95% of cases.
- In a sliding hiatal hernia, the junction where the oesophagus (food pipe) meets the stomach and the upper part of your stomach itself slides up into the chest through the hiatus, which is the opening in the diaphragm.
- This type of hernia is often associated with gastroesophageal reflux disease (GERD) (leaking of acid from your stomach into your oesophagus) because the movement of the stomach into the chest can weaken the lower oesophageal sphincter (LES)(a muscular ring that prevents stomach contents from moving back into the oesophagus), allowing stomach acid to reflux or enter back into the oesophagus.
- Symptoms of a sliding hiatal hernia can include heartburn, acid reflux, regurgitation, chest pain, and difficulty swallowing.
- Paraesophageal Hiatal Hernia:
- Paraesophageal hiatal hernia, also known as a rolling hiatal hernia, is less common but can be more serious than sliding hernias.
- In a paraoesophagheal hiatal hernia, the gastroesophageal junction remains in its normal position, but a portion of your stomach moves through the hiatus and sits beside the oesophagus in the chest cavity.
- Unlike sliding hernias, paraoesophagheal hernias do not typically cause GERD symptoms. Instead, they may lead to symptoms such as chest pain, difficulty swallowing, feeling full quickly, and anaemia due to bleeding from ulcers in the herniated stomach.
Paraoesophageal hernias are also categorised into three subtypes:
- Type I: The gastroesophageal junction remains below the diaphragm, but a portion of the stomach moves into the chest cavity.
- Type II: Similar to Type I, but with the addition of other abdominal organs moving into the chest alongside the stomach.
- Type III: This is the most severe subtype, characterised by the presence of a large portion of the stomach and other abdominal organs moving into the chest cavity.
What are Hiatal Hernia Symptoms?
Hiatal hernia symptoms can vary from person to person but commonly include:
- Heartburn
- Chest pain
- Difficulty swallowing
- Sore throat
- Indigestion
- Burping
- Bad breath
- Dry cough
- Nausea
These symptoms may worsen after eating, lying down, or bending over.
What Causes a Hiatal Hernia?
Hiatal hernias typically happen when there is a weakening or disruption of the muscles and tissues surrounding the hiatus, which is the opening in your diaphragm through which the oesophagus passes before connecting to the stomach.
It is difficult to pinpoint single hiatal hernia causes as several factors such as ageing-related muscle weakening, obesity-induced abdominal pressure, pregnancy-related displacement of organs and hormonal changes, strain from heavy lifting or straining, congenital structural abnormalities, and injury-induced muscle weakening around the hiatus can be listed under hiatal hernia causes.
What are the Risk Factors of Hiatal Hernia?
Several factors increase the risk of developing hiatal hernia, including obesity, advanced age, smoking, and certain medical conditions such as persistent coughing or vomiting. Genetics may also be the risk factor behind this condition.
How is a Hiatal Hernia Diagnosed?
Diagnosing hiatal hernia typically involves a combination of medical history review, physical examination, and diagnostic tests. These hiatal hernia diagnostic tests include:
- Chest X-ray: It also known as a radiograph, utilises radiation to capture static, black-and-white images of the interior of your chest cavity, including the area where your oesophagus is located.
- Upper Endoscopy: In an upper endoscopy, a flexible tube with a camera on the end (endoscope) is inserted through the mouth and into the oesophagus, stomach, and duodenum. This allows your healthcare provider to directly visualise the oesophagus and stomach and identify any abnormalities, such as inflammation or irritation caused by acid reflux.
- Oesophageal pH Monitoring: Oesophageal pH monitoring measures the acidity levels in the oesophagus over a while. This test helps determine the frequency and severity of acid reflux episodes, providing valuable information about the extent of reflux-related symptoms and their impact on oesophageal health.
- Oesophageal Manometry: Oesophageal manometry evaluates the strength and coordination of the muscles in the oesophagus and lower oesophageal sphincter (LES). By measuring muscle contractions and relaxation, this test assesses the functionality of the LES and identifies any abnormalities in oesophageal motility that may contribute to hiatal hernia symptoms.
What is the Treatment for a Hiatal Hernia?
Hiatal hernia treatment aims to relieve symptoms and prevent complications. Depending on the severity of your condition, hiatal hernia treatment options may include medications and surgery.
Medications:
Over-the-counter and prescription hiatal hernia medications such as antacids, proton pump inhibitors (PPIs), and H2-receptor antagonists can help reduce acid production and reduce the symptoms of acid reflux and heartburn.
Surgery:
In cases where medications are ineffective, hiatal hernia surgery may be recommended to repair the hernia and strengthen the lower oesophageal sphincter (a muscular ring that prevents stomach contents from moving back into the oesophagus). Laparoscopic surgery is a minimally invasive approach that offers faster recovery and fewer complications compared to traditional open surgery.
Hiatal Hernia Surgery
Hiatal hernia surgery involves returning the stomach to its normal position and repairing the opening in the diaphragm. This procedure may also involve strengthening your lower oesophageal sphincter to prevent reflux. While recovery times may vary, most hiatal hernia patients can resume normal activities within a few weeks after surgery.
How Can I Treat My Hiatal Hernia at Home?
In addition to medical treatment, certain lifestyle modifications can help manage hiatal hernia symptoms effectively. These hiatal hernia self-care include maintaining a healthy weight, avoiding large meals, elevating the head of the bed while sleeping, and refraining from smoking and excessive alcohol consumption.
Conclusion
Living with hiatal hernia can be challenging, but with proper understanding and management, you can effectively reduce the symptoms and improve your quality of life. Remember to consult with your healthcare provider for personalised treatment recommendations suitable to your individual needs.
At Metropolis Labs, we understand the importance of personalised care and convenience in managing health conditions like hiatal hernia. Our in-house visit services make it easy for you to get the necessary tests done from the comfort of your home, while our informative blogs provide valuable insights into various health topics.













1701259759.webp)









 WhatsApp
WhatsApp