Preventive Healthcare
Dyslipidemia: Symptoms, Causes, Diagnosis, Treatment & Management
4165 Views
0
What is Dyslipidemia?
Dyslipidemia refers to an abnormal level of fats or lipids in the blood. Any lipid parameter, including triglycerides, low-density lipoprotein (LDL) cholesterol, high-density lipoprotein (HDL) cholesterol, or a combination of these lipids, can be affected in dyslipidemia.
Hyperlipidemia, or elevated lipid levels, is the most common form of dyslipidemia. Hypolipidemia, a less common form of dyslipidemia, refers to abnormally low lipid levels. Hypercholesterolemia and hypocholesterolemia describe elevated or decreased cholesterol levels respectively. These may also be referred to as hypolipoproteinemia or hyperlipoproteinemia on occasion. This may be referred to as hypertriglyceridemia (high triglyceride levels) or hypotriglyceridemia (low triglyceride levels) when only triglycerides are affected. On the other hand, a "combined" or "mixed" dyslipidemia occurs when both cholesterol and triglyceride levels are affected.
Dyslipidemia can involve high cholesterol, triglycerides, or low levels of "good" cholesterol (HDL). These abnormal lipid levels contribute to the buildup of plaque in arteries. Dyslipidemia can result in serious issues like heart attack, stroke, type 2 diabetes and other cardiovascular diseases (CVD). Early detection of dyslipidemia allows for early intervention and helps prevent these serious health problems. A lipid panel test is the primary instrument used to evaluate dyslipidemia.
Causes of Dyslipidemia
Several factors, including genetic conditions and lifestyle choices, can cause dyslipidemia. It is classified into two broad categories: Secondary or Primary Dyslipidemia.
- Primary Dyslipidemia: An abnormal level of lipids is referred to as primary dyslipidemia when it is caused by a gene mutation or genes passed down from one or both parents. The term "familial" is used to refer to dyslipidemia that runs in families. People who have primary dyslipidemias with elevated LDL are more likely to develop atherosclerosis early in life, which can cause cardiovascular disease.
Common types of primary dyslipidemias include:
- Familial hypercholesterolemia
- Familial combined hyperlipidemia
- Familial dysbetalipoproteinemia
- Secondary Dyslipidemia: Secondary dyslipidemia is more common and results from lifestyle factors or other medical conditions rather than genetic causes. Factors contributing to secondary dyslipidemia include:
- Poor or high-fat diet
- Diet high in sugar
- Lack of exercise
- Certain medications (e.g., those used to treat HIV, oral contraceptives, antidepressants)
- Liver disease
- Alcohol abuse
- Smoking
- Untreated hypothyroidism
- Uncontrolled diabetes
- Obesity
- Chronic kidney disease
Symptoms of Dyslipidemia
The majority of people with dyslipidemia are unaware they have it unless it is severe. Other conditions, such as coronary artery disease (CAD) and peripheral artery disease (PAD), can result from severe dyslipidemia that is not treated. Heart attacks and strokes are two serious health problems that can arise from both CAD and PAD. In rare cases of extremely high lipids, raised, yellowish bumps known as xanthomas may appear on the body.
These conditions typically exhibit the following symptoms:
- Leg pain (while walking or standing)
- Chest pain
- Chest tightness or pressure
- Shortness of breath
- Pain, tightness, or pressure in the neck, jaw, shoulders, or back
- Indigestion
- Heartburn
- Sleep problems
- Daytime fatigue
- Dizziness
- Palpitations
- Cold sweats
- Vomiting
- Nausea
- Swelling of the veins in the legs, ankles, feet, stomach, or neck
- Fainting
Risk Factors of Dyslipidemia
India has a significantly higher prevalence of dyslipidemia compared to other countries. This condition, often referred to as a "silent killer," can contribute to serious health problems like heart disease and stroke. Here's a closer look at the risk factors:
- Unique Lipid Profile: Studies like the ICMR-INDIAB-17 suggest a unique lipid profile in the Indian population. This may include features like lipid dominance (high triglycerides compared to HDL) and lower HDL cholesterol levels on average. These characteristics necessitate a tailored approach to managing cardiovascular health in India.
- High Prevalence: The ICMR-INDIAB-17 study, published in The Lancet in June 2023, revealed a startling fact: dyslipidemia is more common in India than both diabetes (11.5%) and hypertension (35%). This highlights the importance of early detection and prevention strategies.
- Urbanization: Dyslipidemia rates tend to be higher in urban areas of India. This could be due to factors like dietary changes towards processed foods and reduced physical activity.
- Standard Risk Factors: While India has unique risk factors, several standard risk factors for dyslipidemia also apply:
- Family History: Having a family member with high cholesterol increases your risk.
- Diet: A diet high in saturated and trans fats, refined carbohydrates, and added sugar can contribute to dyslipidemia.
- Weight: Obesity and being overweight are significant risk factors.
- Physical Inactivity: A sedentary lifestyle increases your risk.
- Smoking: Smoking damages blood vessels and increases your risk.
- Medical Conditions: Certain medical conditions like diabetes and hypothyroidism can increase your risk.
Diagnosing Dyslipidemia
There is no real way to know whether you have dyslipidemia - hyperlipidemia or hypolipidemia unless you have a lipid profile done. Your doctor may recommend a blood test more often if you are taking medications for dyslipidemia.
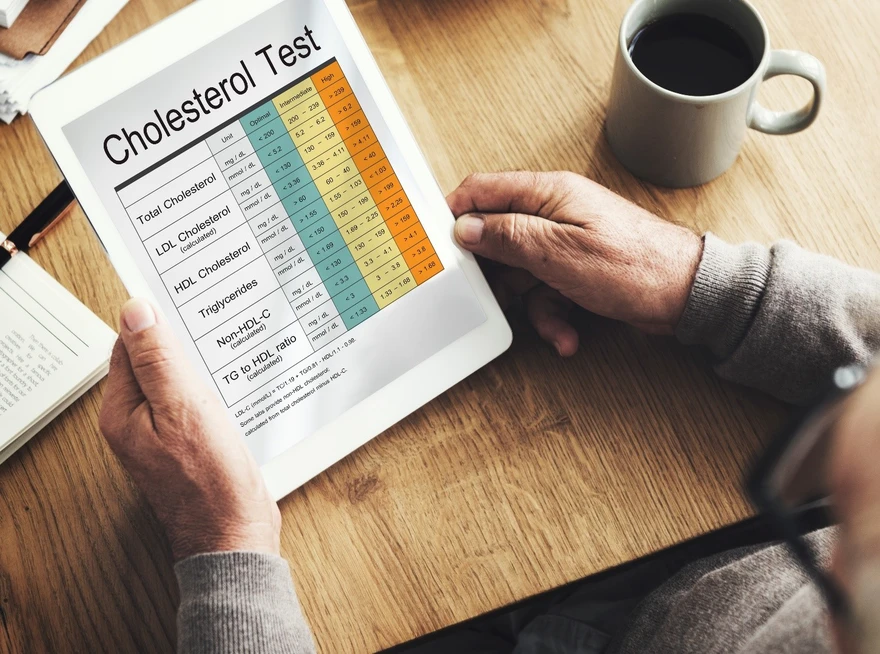
This involves having blood drawn by your healthcare provider and analysed for levels of cholesterol, LDL, HDL, very low-density lipoprotein (VLDL) and triglycerides. Since the LDL, HDL, and triglyceride levels can fluctuate from year to year, an annual blood test is recommended.
New Guidelines in India Put Early Focus on Dyslipidemia Management
India has a high risk of cardiovascular diseases (CVD) compared to other ethnicities, with a significant portion of cases occurring in young adults. Almost half of CVD patients in India are under 50 years old, and about a fifth are younger than 40. The Cardiological Society of India (CSI) has introduced new guidelines to address this specific concern.
The new CSI guidelines focus on two key areas: earlier testing and preventative measures.
- First Lipid Profile at 18: Previously, doctors might wait until midlife to check cholesterol. The new guidelines recommend getting a lipid profile test at the earlier age of 18. This allows for the identification of potential problems early on.
- No Fasting for Most Tests: Traditionally, a lipid profile test required fasting for 10-12 hours beforehand. The new guidelines eliminate this requirement in most cases, making testing more convenient and accessible.
- Lower Targets for Bad Cholesterol: The target LDL cholesterol level for high-risk patients has been lowered to less than 70 mg/dL or non-HDL levels below 85 mg/dL. For extremely high-risk patients, the target is even lower, at less than 55 mg/dL. This more aggressive approach aims to reduce the risk of heart disease more effectively.
Healthy Lipid Levels for General Population in India:
- Total Cholesterol: Less than 200 mg/dL is desirable
- LDL Cholesterol (bad cholesterol):
- Low-risk individuals and the general population: Below 130 mg/dL
- High-risk individuals (diabetes, hypertension): Below 100 mg/dL
- HDL Cholesterol (good cholesterol): 60 mg/dL or higher is desirable
- Triglycerides: Less than 150 mg/dL is desirable
The new dyslipidemia guidelines in India are a positive step towards preventing heart disease. By getting screened earlier and adopting healthy lifestyle habits, you can significantly reduce your risk. Talk to your doctor about your individual risk factors and create a personalized plan to keep your heart healthy.
Treatment of Dyslipidemia
Fortunately, dyslipidemia is a treatable condition. Various treatments and other measures are available to address dyslipidemia. Lifestyle changes are a cornerstone of treatment, including:
- Reducing sugar and carbohydrate intake: A diet lower in sugary drinks, refined carbohydrates, and saturated fats can significantly improve cholesterol levels.
- Regular exercise: Aim for at least 30 minutes of moderate-intensity exercise most days of the week. Activities like brisk walking, cycling, or swimming are all beneficial.
- Quitting smoking
- Addressing any medical conditions that may be causing high lipid levels.
In some cases, medications are also used to lower your lipid levels and reduce your risk of future heart disease.
- Statins: These drugs are the mainstay of medication treatment for high cholesterol.
- Oral non-statin medications: These medications can be used alone or in combination with statins to lower cholesterol and triglycerides.
Prevention Tips for Dyslipidemia
The good news is that you have significant power to prevent or manage dyslipidemia. Here are some key strategies:
Lifestyle Changes:
- Eat Heart-Healthy: Focus on a diet rich in fruits, vegetables, whole grains, and lean protein sources like fish, poultry, and beans. Limit saturated and trans fats found in red meat, processed foods, and fried foods.
- Move Your Body: Aim for at least 30 minutes of moderate-intensity exercise most days of the week. Activities like brisk walking, cycling, swimming, or dancing are all excellent choices.
- Manage Weight: Maintaining a healthy weight can significantly improve your cholesterol profile. If you're overweight or obese, talk to your doctor about healthy weight loss strategies.
- Quit Smoking: Smoking damages blood vessels and contributes to dyslipidemia. Quitting smoking is one of the most impactful ways to improve your heart health.
- Manage Stress: Chronic stress can raise blood pressure and negatively impact cholesterol levels. Explore stress-reduction techniques like yoga, meditation, or deep breathing exercises.
Dietary Tweaks:
- Limit Alcohol: Excessive alcohol consumption can raise triglycerides. Talk to your doctor about a healthy level of alcohol intake for you.
- Reduce Sugary Drinks and Refined Carbs: Sugary drinks and refined carbohydrates like white bread and pastries can contribute to unhealthy cholesterol levels. Opt for water and whole grains instead.
Early Detection and Management:
- Talk to Your Doctor: Discuss your risk factors for dyslipidemia with your doctor and get screened at the recommended age of 18.
- Non-Fasting Lipid Tests: The new guidelines recommend non-fasting lipid profile tests in most cases, making testing more convenient.
- Family History: If you have a family history of high cholesterol, be proactive about healthy lifestyle habits.
By following these tips, you can significantly reduce your risk of dyslipidemia and protect your heart health for years to come. Remember, early detection and intervention are crucial. Talk to your doctor to develop a personalized prevention plan based on your individual risk factors.























 WhatsApp
WhatsApp