Preventive Healthcare
Understanding Hypoxemia: Symptoms, Causes and Treatments
Table of Contents
- What is the definition of hypoxemia?
- Hypoxia vs Hypoxemia: What's the Difference?
- Who Does Hypoxemia Affect?
- What are the symptoms of hypoxemia?
- What is the most common cause of hypoxemia?
- What are the five causes of hypoxemia?
- How is hypoxemia diagnosed?
- How is hypoxemia treated?
- How do I manage the symptoms of hypoxemia?
- What are the complications or side effects of hypoxemia?
- How can I reduce my risk of hypoxemia?
- How can I raise my oxygen level?
- When to see a doctor?
- What questions should I ask my doctor about hypoxemia?
- Conclusion
Taking charge of your health can be overwhelming, but knowledge is a powerful tool. Understanding conditions like hypoxemia is crucial for your well-being. Recognizing the signs of hypoxemia is crucial for early intervention. Hypoxemia symptoms include shortness of breath, rapid breathing, confusion, chest pain, and bluish discolouration of the skin. By being aware of these indicators, individuals can seek medical attention promptly, preventing further deterioration of their health.
What is the definition of hypoxemia?
Hypoxemia definition: Hypoxemia is a medical condition characterised by low levels of oxygen in the blood. This can result from various factors affecting the respiratory or circulatory systems.
Hypoxemia symptoms include shortness of breath, confusion, and changes in skin colour from blue to cherry red. Rapid heart rate and breathing are common indicators.
The causes of hypoxemia include respiratory disorders like asthma, pneumonia, or chronic obstructive pulmonary disease (COPD). Additionally, issues with blood circulation, such as heart failure, can contribute to inadequate oxygen delivery to tissues.
Hypoxemia is diagnosed through blood tests measuring oxygen saturation levels. Hypoxemia treatment involves addressing the underlying cause, such as administering supplemental oxygen, bronchodilators, or addressing circulatory issues. Severe cases may require hospitalisation.
It's crucial to note that hypoxemia is related to but distinct from hypoxia. While hypoxemia refers specifically to low blood oxygen levels, hypoxia encompasses low oxygen levels in tissues. Both conditions need proper medical intervention.
Hypoxia vs Hypoxemia: What's the Difference?
Hypoxemia and hypoxia are related but distinct terms in the context of oxygen levels in the body:
- Hypoxemia: Refers to low oxygen levels in the blood. It is measured by the partial pressure of oxygen in arterial blood (PaO2) and can result from issues like respiratory disorders or poor lung function. Hypoxemia levels do not necessarily indicate low oxygen in tissues.
- Hypoxia: This means low oxygen levels in bodily tissues. It reflects inadequate oxygen supply to cells and organs. Hypoxia can occur even if blood oxygen levels are normal, as it involves the ability of tissues to utilise oxygen. Causes include circulatory problems or anaemia.
Who Does Hypoxemia Affect?
Hypoxemia can affect individuals of all ages and backgrounds, and its impact is often associated with underlying health conditions or environmental factors.
- Individuals with Respiratory Conditions: People with chronic respiratory conditions such as asthma, chronic obstructive pulmonary disease (COPD), or pneumonia are at a higher risk of hypoxemia due to compromised lung function.
- Cardiovascular Patients: Those with heart-related issues, including heart failure or coronary artery disease, may experience hypoxemia due to reduced oxygenated blood circulation.
- Smokers: Smoking damages the lungs and can contribute to respiratory problems, increasing the risk of hypoxemia.
- Elderly Individuals: Aging often comes with a decline in lung and cardiovascular function, making older adults more susceptible to hypoxemia.
- Patients in Intensive Care: Individuals in critical care units, especially those on mechanical ventilation, may be prone to hypoxemia.
- High-altitude Dwellers: Living at high altitudes with lower oxygen levels in the atmosphere can lead to chronic hypoxemia over time.
What are the symptoms of hypoxemia?
Hypoxemia symptoms, indicative of low blood oxygen levels, can vary in severity. Common hypoxemia symptoms include:
- Shortness of Breath: Feeling breathless or having difficulty breathing, especially during physical activity.
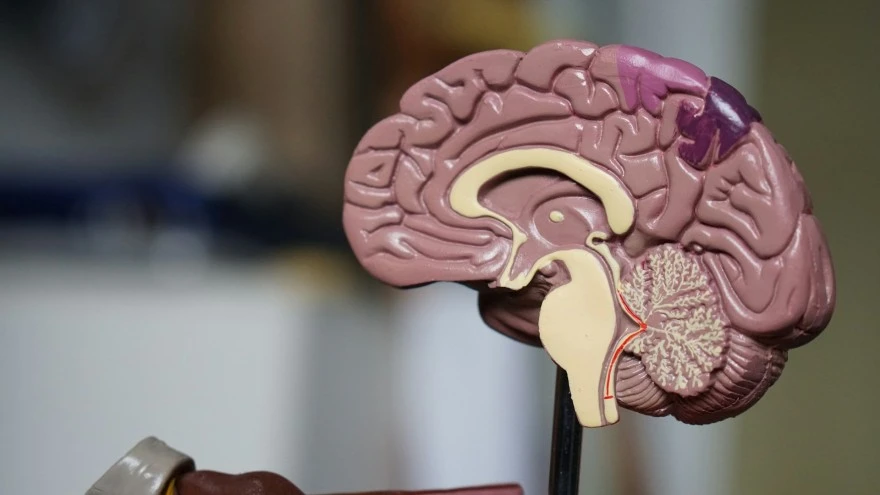
- Confusion: Cognitive impairment and confusion can result from inadequate oxygen reaching the brain.
- Changes in Skin Colour: Skin may appear bluish or even cherry red, indicating poor oxygen level.
- Rapid Heart Rate: An increased heart rate is the body's response to oxygen deprivation.
- Rapid Breathing: Shallow or faster breathing is a compensatory mechanism to enhance oxygen intake.
- Cough: In some cases, hypoxemia may cause a persistent cough.
What is the most common cause of hypoxemia?
The most common cause of hypoxemia is impaired gas exchange in the lungs, often associated with respiratory disorders. Key hypoxemia causes include:
- Carbon Monoxide Poisoning: Inhalation of carbon monoxide, often due to exposure to smoke from fires or malfunctioning heating systems, can lead to the formation of carboxyhemoglobin, reducing the blood's ability to transport oxygen.
- Neuromuscular Disorders: Conditions that affect the nerves and muscles involved in breathing, such as amyotrophic lateral sclerosis (ALS) or Guillain-Barré syndrome, can result in inadequate ventilation and contribute to hypoxemia.
- Pulmonary Hypertension: Elevated blood pressure in the pulmonary arteries can lead to increased resistance and strain on the right side of the heart, affecting its ability to pump blood to the lungs for oxygenation.
- ARDS (Acute Respiratory Distress Syndrome): ARDS can be caused by severe infections, trauma, or other lung injuries. It leads to inflammation in the lungs, impaired gas exchange, and ultimately hypoxemia.
- Interstitial Lung Disease: Various forms of interstitial lung disease, characterized by inflammation and scarring of lung tissue, can result in decreased lung compliance and impaired oxygenation.
What are the five causes of hypoxemia?
Hypoxemia, characterised by low oxygen levels in the blood, can result from various underlying factors. Here are five common hypoxemia causes:
- Respiratory Disorders: Chronic respiratory conditions significantly contribute to hypoxemia. Diseases such as chronic obstructive pulmonary disease (COPD), asthma, pneumonia, and interstitial lung diseases can impair the lungs' ability to adequately exchange oxygen and carbon dioxide.
- Ventilation-Perfusion Mismatch: The efficient exchange of oxygen and carbon dioxide relies on a balance between ventilation (airflow in the lungs) and perfusion (blood flow in the pulmonary vessels). Mismatch in this balance, caused by conditions like pulmonary embolism or chronic bronchitis, can lead to areas of the lungs receiving insufficient oxygen, contributing to hypoxemia.
- Cardiovascular Issues: Heart-related conditions can affect the circulation of oxygenated blood throughout the body, leading to hypoxemia. Heart failure, congenital heart diseases, and conditions that compromise blood vessel integrity can contribute to inadequate oxygen delivery to tissues.
- Hypoventilation: Inadequate ventilation, where breathing is insufficient to meet the body's oxygen demands, is another one of hypoxemia causes. Conditions such as sleep apnoea, respiratory muscle weakness, or drug-induced respiratory depression can result in reduced oxygen intake.
- High Altitude Living: Living at high altitudes, where the atmospheric oxygen concentration is lower, can lead to chronic hypoxemia. At higher elevations, the partial pressure of oxygen in the air decreases, making it more challenging for individuals to maintain adequate blood oxygen levels.
How is hypoxemia diagnosed?
Diagnosing hypoxemia involves a comprehensive approach, including medical history, physical examination, and various tests:
- Medical History and Physical Exam: Healthcare providers assess hypoxemia symptoms, risk factors, and overall health. Physical examinations help identify signs like changes in skin colour or respiratory distress.
- Arterial Blood Gas (ABG) Test: This blood test measures oxygen and carbon dioxide levels in arterial blood, providing information about oxygen saturation and the partial pressure of oxygen (PaO2).
- Pulse Oximetry: A non-invasive test that measures oxygen saturation in the blood by attaching a small sensor to a fingertip or earlobe.
- Imaging Studies: Chest X-rays or CT scans can reveal lung abnormalities, helping identify conditions contributing to hypoxemia.
- Lung Function Tests: Assess lung capacity and function, helping diagnose respiratory disorders affecting oxygen exchange.
- A-a Gradient Calculation: The Alveolar-arterial (A-a) gradient measures the difference in oxygen concentration between the alveoli and arterial blood. Elevated levels may indicate hypoxemia.
- Cardiac Evaluations: Assessing heart function is crucial, as cardiovascular issues can contribute to inadequate oxygen delivery.
- Sleep Studies: In cases of suspected sleep apnoea, studies like polysomnography can identify nighttime hypoxemia.
- Exercise Testing: Evaluating oxygen levels during physical activity helps assess the impact of exertion on oxygenation.
- Ventilation-Perfusion (V/Q) Scans: These nuclear medicine scans assess lung ventilation and blood perfusion, aiding in identifying areas with impaired oxygen exchange.
How is hypoxemia treated?
The hypoxemia treatment aims to improve oxygen levels in the blood and address the underlying cause. Key interventions and hypoxemia treatment include:
- Supplemental Oxygen Therapy: Administering additional oxygen through various devices like nasal cannulas, masks, or high-flow nasal cannulas helps raise oxygen levels in the blood and alleviate hypoxemia symptoms.
- High-flow Nasal Cannula (HFNC): HFNC delivers humidified and heated oxygen at higher flow rates than traditional devices, providing better comfort and oxygenation, particularly in respiratory distress situations.
- Emergency Oxygen Therapy: Guided by prescribed target saturation ranges, emergency oxygen therapy corrects hypoxemia. Oxygen is considered a drug and should be administered with attention to dosages and patient response.
- Management of Underlying Conditions: Treating the root cause, such as respiratory or cardiovascular disorders, is essential for long-term management and prevention of hypoxemia recurrence.
- Ventilation Support: In severe cases, mechanical ventilation may be necessary to assist with breathing and ensure adequate oxygenation.
- Positioning and Mobilisation: Optimising the patient's position and encouraging mobility can enhance lung function and oxygen exchange.
- Continuous Monitoring: Regular monitoring of oxygen saturation levels, respiratory rate, and clinical signs guides the adjustment of hypoxemia treatment strategies.
How do I manage the symptoms of hypoxemia?
Managing hypoxemia symptoms involves addressing the underlying cause and improving oxygen levels. Key steps include:
- Supplemental Oxygen: Administering additional oxygen through devices like nasal cannulas or masks.
- Treating Underlying Conditions: Addressing respiratory or cardiovascular issues contributing to hypoxemia.
- Positioning: Optimising patient positioning to enhance breathing and oxygenation.
- Mobility: Encouraging movement to improve lung function and oxygen exchange.
- Continuous Monitoring: Regularly assessing oxygen levels, respiratory rate, and clinical signs for prompt adjustments.
What are the complications or side effects of hypoxemia?
Hypoxemia, or low blood oxygen levels, can lead to various complications and side effects, including:
- Organ Dysfunction: Severe hypoxemia may impair organ function, particularly in the brain, causing restlessness, confusion, and headache.
- Cardiovascular Effects: Hypoxemia can strain the cardiovascular system, leading to a rapid heartbeat and increased cardiac workload.
- Respiratory Distress: Shortness of breath, rapid breathing, and laboured breathing are common hypoxemia symptoms, indicating the respiratory system's struggle to maintain adequate oxygen levels.
- Neurological Manifestations: Hypoxemia may manifest neurologically with hypoxemia symptoms like irritability, confusion, and muscle twitching.
- Tissue Damage: Prolonged hypoxemia can lead to cell and tissue damage due to insufficient oxygen supply.
How can I reduce my risk of hypoxemia?
To reduce the risk of hypoxemia, consider the following measures:
- Maintain Good Respiratory Health: Practice regular deep breathing exercises and maintain overall lung health.
- Avoid Smoking: Smoking damages the lungs and can contribute to respiratory issues; quitting smoking reduces the risk.
- Monitor Altitude Exposure: Be cautious at high altitudes, where oxygen levels are lower; acclimatise gradually.
- Manage Chronic Conditions: Effectively manage chronic respiratory conditions like COPD or asthma with proper medical guidance.
- Exercise Regularly: Physical activity improves lung function and overall cardiovascular health.
- Adhere to Oxygen Therapy: If prescribed, adhere to oxygen therapy recommendations, especially in chronic respiratory conditions.
- Stay Hydrated: Maintain adequate hydration to support overall physiological function.
How can I raise my oxygen level?
To naturally raise your blood oxygen level, consider the following tips:
- Practice Breathing Exercises: Engage in deep breathing exercises like pursed-lip breathing and deep belly breathing to enhance lung function and oxygen intake.
- Lie Down in the Prone Position: The prone position, lying face down, is recommended to boost oxygen levels in your body
- Get Fresh Air: Spend time in well-ventilated areas and breathe in fresh air to elevate blood oxygen levels.
- Stay Hydrated: Proper hydration supports efficient lung function, aiding in oxygen dispersion into the bloodstream.
- Include Antioxidant-rich Foods: Consume foods high in antioxidants, such as lemons, turmeric, spinach, grapes, avocados, and nuts, to promote oxygenation.
- Quit Smoking: If you smoke, quitting is essential, as smoking impairs lung function and hinders oxygen absorption.
- Maintain Good Hygiene: Proper lung hygiene, including avoiding exposure to pollutants, contributes to respiratory health.
When to see a doctor?
If you or someone else is exhibiting signs of hypoxemia, it is crucial to seek immediate medical attention. Hypoxemia symptoms include severe trouble breathing, a very rapid heart rate, discoloured skin, or altered levels of consciousness. These indicate a potential lack of oxygen in the body, requiring prompt evaluation by a healthcare professional.
What questions should I ask my doctor about hypoxemia?
When discussing hypoxemia with your doctor, consider asking the following questions:
- What is causing my hypoxemia? Seek clarification on the underlying reasons for your low blood oxygen levels.
- What tests are needed for diagnosis? Inquire about diagnostic procedures to better understand your condition.
- What are the hypoxemia treatment options? Discuss available therapies, including medications or oxygen therapy.
- Are there lifestyle changes I should make? Explore any modifications to improve your overall health and manage hypoxemia.
- What are the potential complications? Understand the risks and complications associated with untreated hypoxemia.
- How can I monitor my oxygen levels at home? Learn about tools or devices for monitoring blood oxygen levels outside the medical setting.
- What should I do in case of worsening Hypoxemia symptoms? Establish a plan for managing and responding to any deterioration in your condition.
Conclusion
Understanding hypoxemia is crucial for maintaining overall health. Recognising hypoxemia causes and hypoxemia symptoms helps individuals to take proactive steps towards effective management. Whether it's lifestyle adjustments or medical interventions, early detection and intervention are key.
Get yourself tested at Metropolis Labs. Our skilled team of technicians offers easy at-home sample collection. Above all, you can access your reports hassle-free through email or the user-friendly Metropolis TruHealth app.