Preventive Healthcare
Allergic Bronchopulmonary Aspergillosis (ABPA): Causes, Symptoms, and Treatment
4228 Views
0
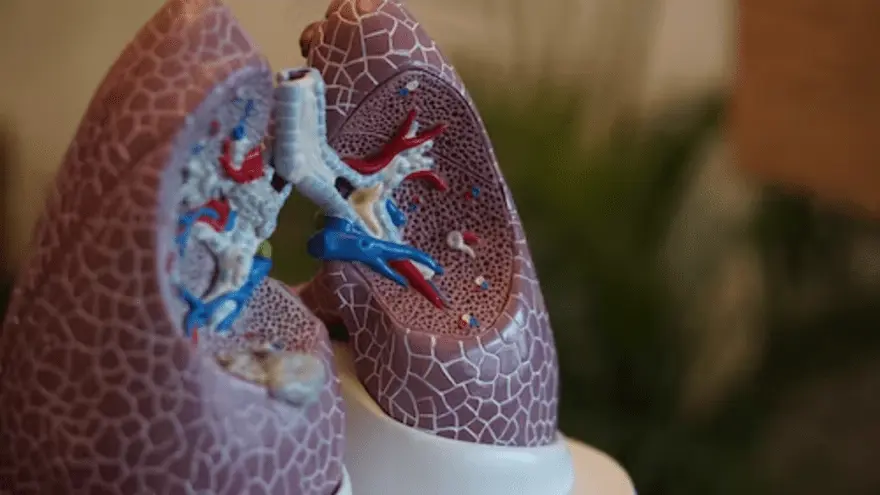
Allergic Bronchopulmonary Aspergillosis, or ABPA, is a relatively rare but potentially serious respiratory condition that often goes undiagnosed.
Whether you're someone dealing with respiratory issues or simply curious about this condition, we will delve into the details to help you better understand ABPA and its implications on respiratory health. This blog will delve into various aspects of ABPA, from its causes and symptoms to diagnosis with abpa tests and treatment.
What is Aspergillus?
Aspergillus is a genus of fungi that includes a wide variety of species. These fungi are commonly found in both indoor and outdoor environments. Aspergillus species are characterised by their ability to produce airborne spores called conidia, which can be easily inhaled by humans and animals.
Aspergillus can cause various health issues, particularly respiratory infections and allergies. The most well-known condition associated with Aspergillus is Aspergillosis, which refers to a group of fungal infections caused by different species of Aspergillus. Aspergillosis can affect the respiratory system and other parts of the body, leading to a range of aspergillosis symptoms and complications.
It's important to note that while many people are exposed to Aspergillus spores in the environment, they may not necessarily develop infections. However, individuals with weakened immune systems or underlying respiratory conditions, such as asthma or cystic fibrosis, are more susceptible to Aspergillus-related health problems.
What is ABPA?
ABPA, or Allergic Bronchopulmonary Aspergillosis, is a complex respiratory condition characterised by an overactive immune response to Aspergillus fungi, which are commonly found in the environment. This exaggerated hypersensitivity reaction primarily affects the lungs and is typically seen in individuals with underlying respiratory conditions, such as asthma or cystic fibrosis.
Common symptoms of ABPA include persistent wheezing, coughing, shortness of breath, chest pain, and the production of thick, sticky mucus. Some individuals with ABPA may also develop a fever.
Over time, if left untreated, ABPA can lead to lung damage and impaired respiratory function. Therefore, early diagnosis and management are crucial in controlling ABPA and preventing long-term complications. Treatment typically involves a combination of antifungal medications to target the Aspergillus fungi and corticosteroids to reduce inflammation.
Close monitoring by doctors is essential for individuals with ABPA, especially those with underlying respiratory conditions, to improve their quality of life and minimise the impact of this hypersensitivity reaction on their lung health.
Common Signs and Symptoms of ABPA
Common signs and symptoms of Allergic Bronchopulmonary Aspergillosis (ABPA) include:
Respiratory symptoms:
- Wheezing: Individuals with ABPA often experience wheezing, which is a high-pitched whistling sound when breathing.
- Cough: A persistent cough is a common symptom of ABPA.
- Shortness of breath: People with ABPA may have difficulty breathing, especially during physical activity.
- Chest pain or tightness: Some individuals report chest discomfort or a feeling of tightness.
Coughing with bloody sputum:
- ABPA can lead to the production of mucus plugs that may contain blood, leading to coughing with bloody sputum.
General systemic symptoms:
- Fever: In severe cases, individuals with ABPA may experience fever.
- Headache: Some patients may have headaches.
- Anorexia: Loss of appetite and decreased food intake can occur.
- Fatigue: ABPA may cause fatigue, leading to a lack of energy.
- Generalised aches and pains: Some individuals may experience body aches and pains.
Airway obstruction:
- ABPA causes bronchospasm, which is the tightening of airway muscles, leading to airway obstruction. This can aggravate symptoms like wheezing and difficulty breathing.
ABPA with Asthma
It's crucial to manage asthma and Allergic Bronchopulmonary Aspergillosis (ABPA) when they affect a person at the same time. Effective treatment is essential for symptom control and preventing exacerbations in individuals with both conditions.
Additionally, conducting an ABPA test is essential for accurate ABPA diagnosis and tailored management. Early detection through appropriate testing allows doctors to implement targeted treatment strategies, ultimately enhancing the patient's overall well-being.
ABPA with Cystic Fibrosis (CF)
Managing both cystic fibrosis and Allergic Bronchopulmonary Aspergillosis (ABPA) in patients with cystic fibrosis is crucial. A comprehensive, multidisciplinary approach is necessary to effectively address the challenges that arise when these conditions coexist.
An ABPA blood test, also known as an IgE antibodies to Aspergillus test, is used to detect sensitisation to Aspergillus fungus, which is essential in diagnosing Allergic Bronchopulmonary Aspergillosis (ABPA).
ABPA blood tests are part of the diagnostic criteria for ABPA and involve measuring specific IgE antibodies to Aspergillus in the bloodstream, especially in individuals with predisposing conditions like asthma or cystic fibrosis
How do I Know if I Have ABPA?
Diagnosing Allergic Bronchopulmonary Aspergillosis (ABPA) is complex due to its similar symptoms to other lung conditions. Here's how the abpa test is done:
- Clinical evaluation: Doctors start by asking about symptoms like wheezing, coughing, shortness of breath, and mucus production. They consider if you have asthma or cystic fibrosis, as ABPA is common in those with these conditions.
- Imaging studies: Chest X-rays and CT scans show lung issues caused by Aspergillus fungi, such as infiltrates, widened airways (bronchiectasis), and mucus blockages.
- Pulmonary function ABPA tests: Spirometry measures lung function. ABPA can reduce airflow, lung capacity, and gas exchange, which these ABPA panel tests detect.
- Laboratory tests: abpa panel tests like blood tests check for specific IgE antibodies against Aspergillus, showing sensitivity to the fungus. High eosinophil levels (allergy-related white blood cells) and precipitins (antibodies against Aspergillus) confirm ABPA.
- Sputum culture: In complex cases, a sputum culture isolates Aspergillus from respiratory secretions, helping with a definitive diagnosis.
- Bronchoscopy: Sometimes, a bronchoscopy with a tiny camera is done to directly view airway issues and collect samples for testing.
- ABPA screen test: The ABPA screen test is a preliminary diagnostic tool used to assess whether an individual might be sensitised to Aspergillus and at risk of developing ABPA.
An ABPA test typically involves the measurement of specific antibodies, such as IgE antibodies, to Aspergillus, a fungus that can trigger allergic reactions in individuals with ABPA.
An ABPA test helps in diagnosing the condition by identifying an elevated level of these antibodies, indicating sensitisation or an allergic response to Aspergillus. The ABPA test aids doctors in confirming the presence of ABPA and guiding appropriate treatment.
How is ABPA Treated?
The treatment of Allergic Bronchopulmonary Aspergillosis (ABPA) typically involves a combination of medications and management strategies. Here's an overview of how ABPA treatment:
Systemic glucocorticoids (steroids):
- Systemic glucocorticoids, such as prednisone, are often used as the first-line treatment for ABPA. They help reduce inflammation and control the immune response to Aspergillus.
- Steroids are usually prescribed in high doses initially to manage acute symptoms.
Antifungal therapy:
- Antifungal medications are commonly used to combat the Aspergillus infection. Itraconazole is recommended for patients who are dependent on steroids or have frequent acute episodes of ABPA.
- Antifungal therapy helps to control the growth of Aspergillus fungi in the respiratory tract.
Monitoring:
- Regular monitoring of lung function and symptoms is essential to assess treatment effectiveness and disease progression.
- Imaging studies like chest X-rays and CT scans may be used to evaluate the lungs.
Biologic therapy:
- Omalizumab, a biologic therapy, can be an option for severe or refractory Allergic Bronchopulmonary Aspergillosis (ABPA). It specifically targets the immune responses associated with ABPA.
Lifestyle management:
- Avoiding exposure to environmental allergens, including Aspergillus spores, can help reduce the risk of exacerbations.
- Proper asthma management, including the use of bronchodilators and inhaled corticosteroids, is important for individuals with asthma and ABPA.
Education and patient support:
- Patient education about ABPA, its triggers, and the importance of sticking to treatment plans is crucial.
- Support from healthcare providers, such as pulmonologists and allergists, can help individuals manage ABPA effectively.
ABPA life expectancy:
- Allergic Bronchopulmonary Aspergillosis (ABPA) has a variable impact on life expectancy. Proper medical management can help individuals lead normal lives, but untreated ABPA may lead to lung damage and reduced life expectancy.
Conclusion
Allergic Bronchopulmonary Aspergillosis (ABPA) is a complex respiratory condition caused by hypersensitivity to Aspergillus fungi, primarily affecting those with asthma or cystic fibrosis. Timely diagnosis and proper treatment are important in managing ABPA and enhancing patients' lives. If you suspect ABPA or have been diagnosed, consult a doctor for personalised care.
For comprehensive diagnostic services, consider Metropolis Labs, a trusted chain of diagnostic labs across India. Their skilled blood collection technicians offer convenient at-home sample collection. Advanced labs process samples and reports are easily accessible online via email and the Metropolis TruHealth app.























 WhatsApp
WhatsApp